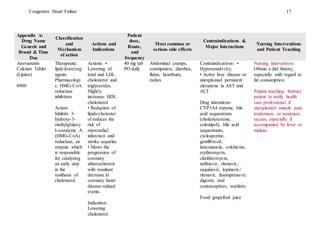
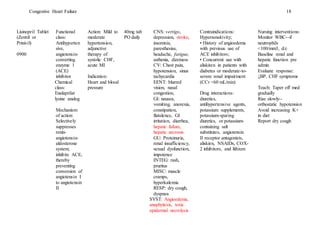
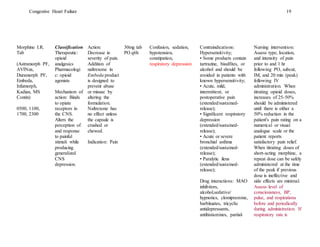
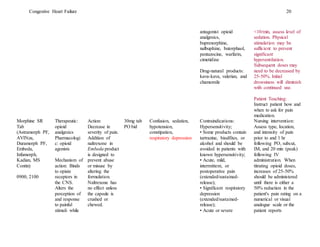
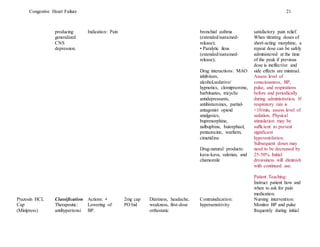
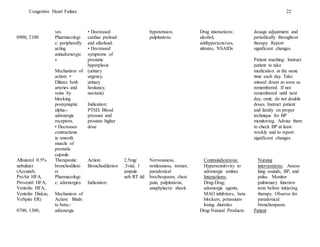
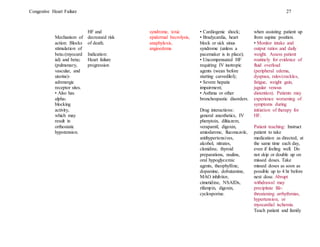
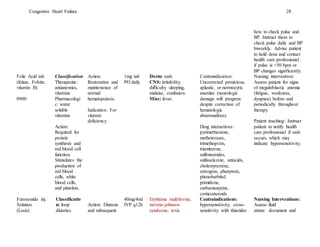
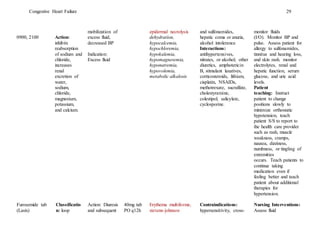
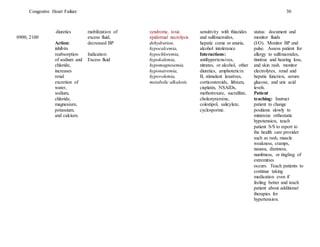
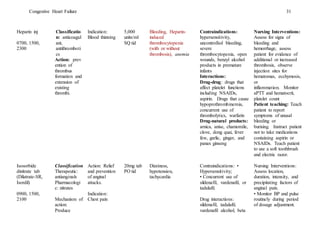
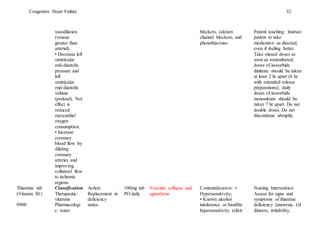
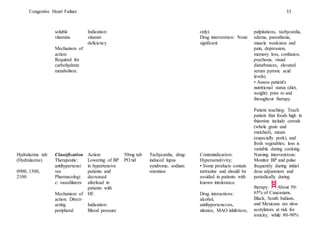
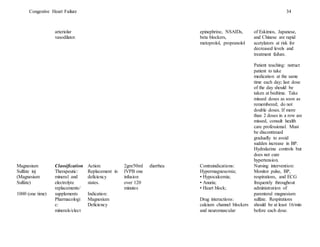
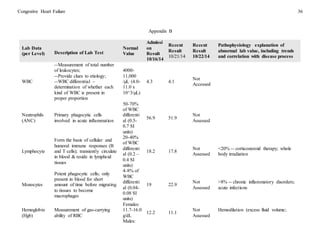
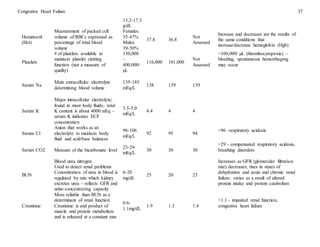
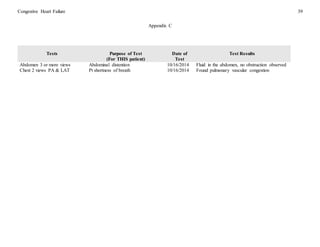
This document provides a case study of a 65-year-old African American male patient diagnosed with congestive heart failure (CHF). It describes the patient's medical history and symptoms, including shortness of breath, weight gain, and leg edema. Diagnostic tests confirmed pulmonary congestion and excess fluid in the abdomen. The patient has multiple comorbidities and takes medications to treat CHF including ACE inhibitors, beta-blockers, and diuretics. Nursing diagnoses focus on impaired gas exchange and excess fluid volume related to CHF. Interventions target monitoring oxygen levels, reducing sodium intake, and administering diuretics to decrease edema.