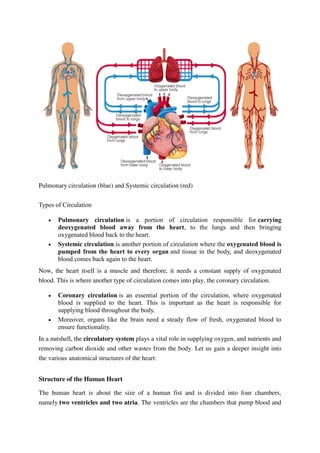
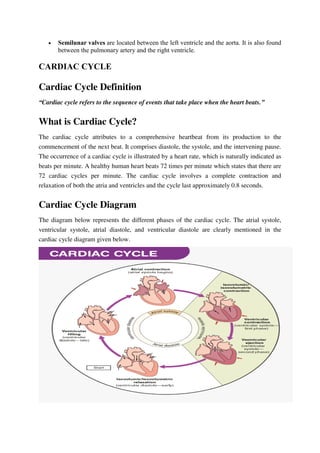
The cardiovascular system consists of the heart and blood vessels. The heart is a muscular organ located in the chest that pumps blood through the body in a process called circulation. It has four chambers - two atria that receive blood and two ventricles that pump blood. The heart functions throughout life to circulate oxygenated blood from the lungs and nutrients throughout the body via two types of circulation - pulmonary and systemic. The cardiac cycle describes the repeating sequence of heart contraction and relaxation that pumps blood through the circulatory system.