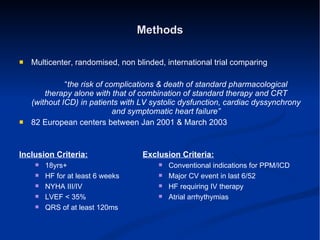
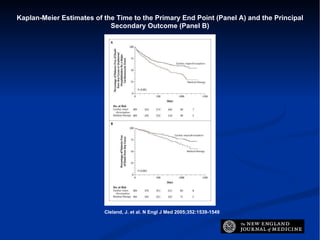
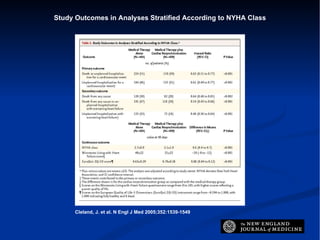
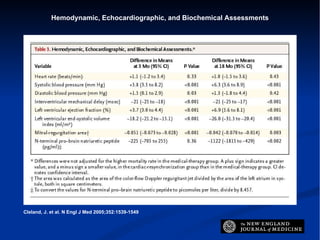
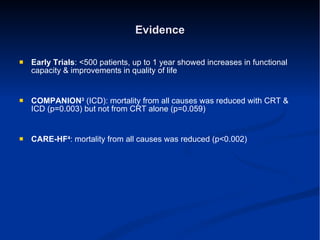
This document summarizes the results of the CARE-HF trial, which investigated the effects of cardiac resynchronization therapy (CRT) in patients with heart failure. The trial found that CRT significantly reduced the risks of death and hospitalization compared to medical therapy alone. For every 9 patients treated with CRT, 1 death and 3 hospitalizations were prevented. The results provide strong evidence that CRT can reduce both morbidity and mortality in patients with moderate to severe heart failure.