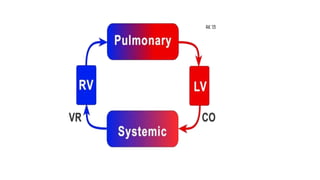
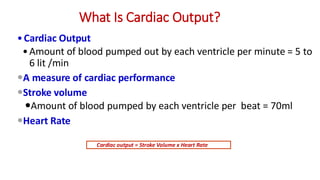
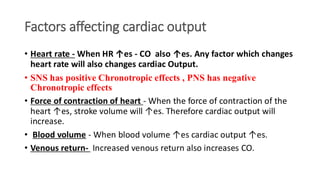
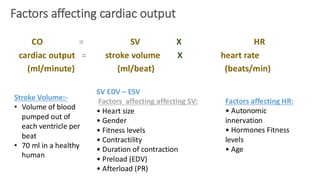
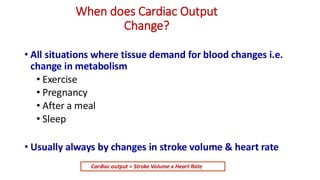
The document provides an overview of cardiac output, detailing its definition, measurement, and factors influencing it such as heart rate and stroke volume. It also discusses methods for measuring cardiac output, the role of ECG in cardiac assessment, and the classification and implications of shock. Key topics include physiological and pathological factors affecting cardiac output, the significance of heart rate, and the importance of various measurement techniques.