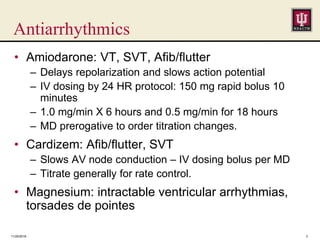
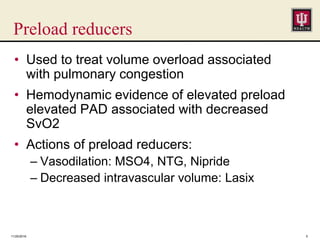
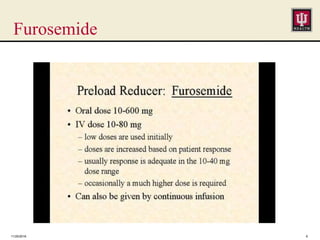
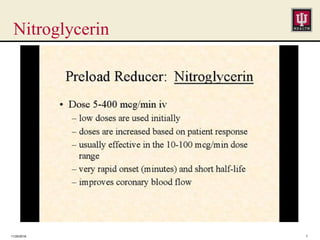
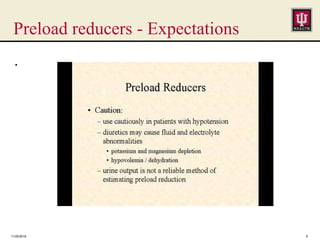
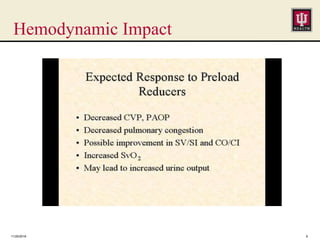
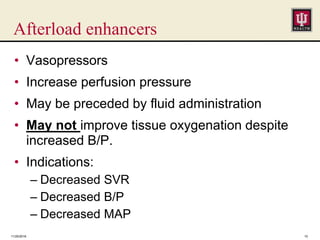
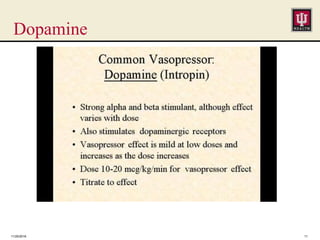
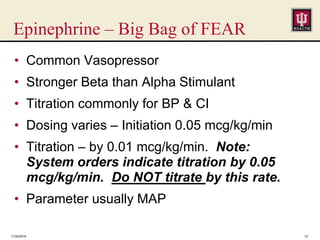
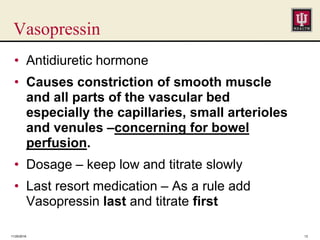
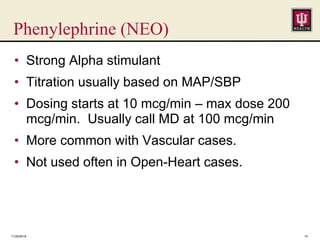
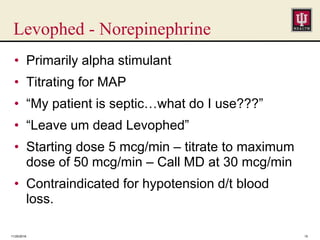
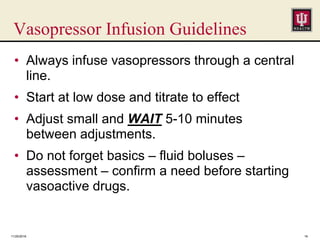
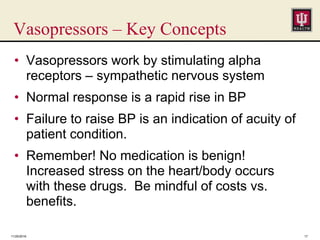
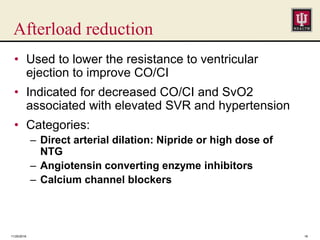
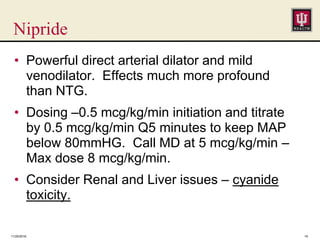
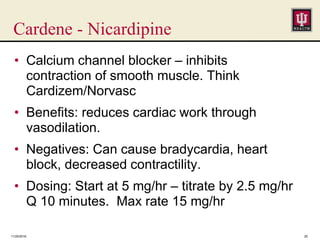
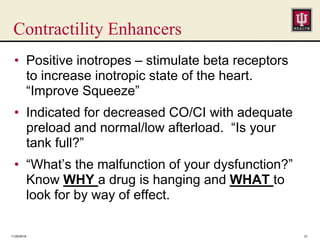
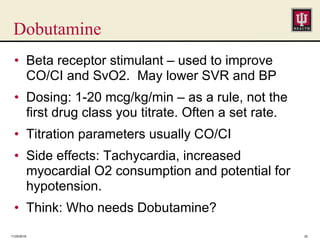
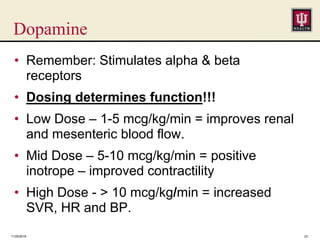
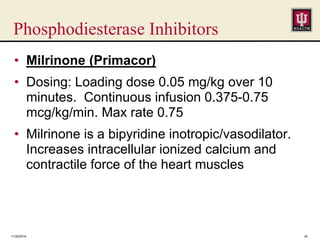
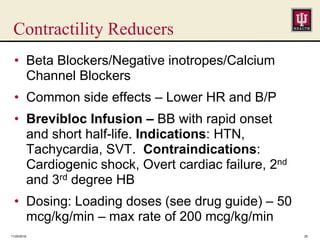
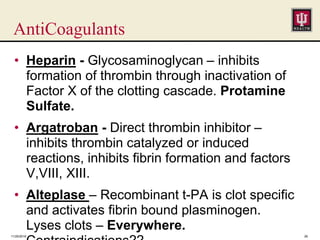
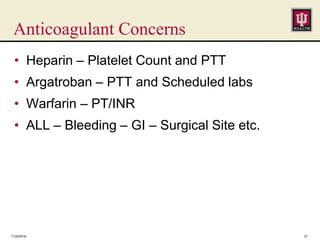
This document provides an overview of various cardiovascular medications, including their uses, dosages, and key effects. It discusses medications that alter hemodynamics such as heart rate, preload, afterload, and contractility. Specific drugs covered include antiarrhythmics like amiodarone and diltiazem, preload enhancers and reducers, vasopressors like dopamine and epinephrine, afterload reducers like nitroprusside, inotropes like dobutamine, and anticoagulants like heparin. Important considerations for each drug class and specific medications are outlined, such as dosing protocols, hemodynamic impacts, and monitoring parameters.