The document discusses various medical topics including:
- The three main measurement systems used in clinical practice.
- Components of a health history and physical examination.
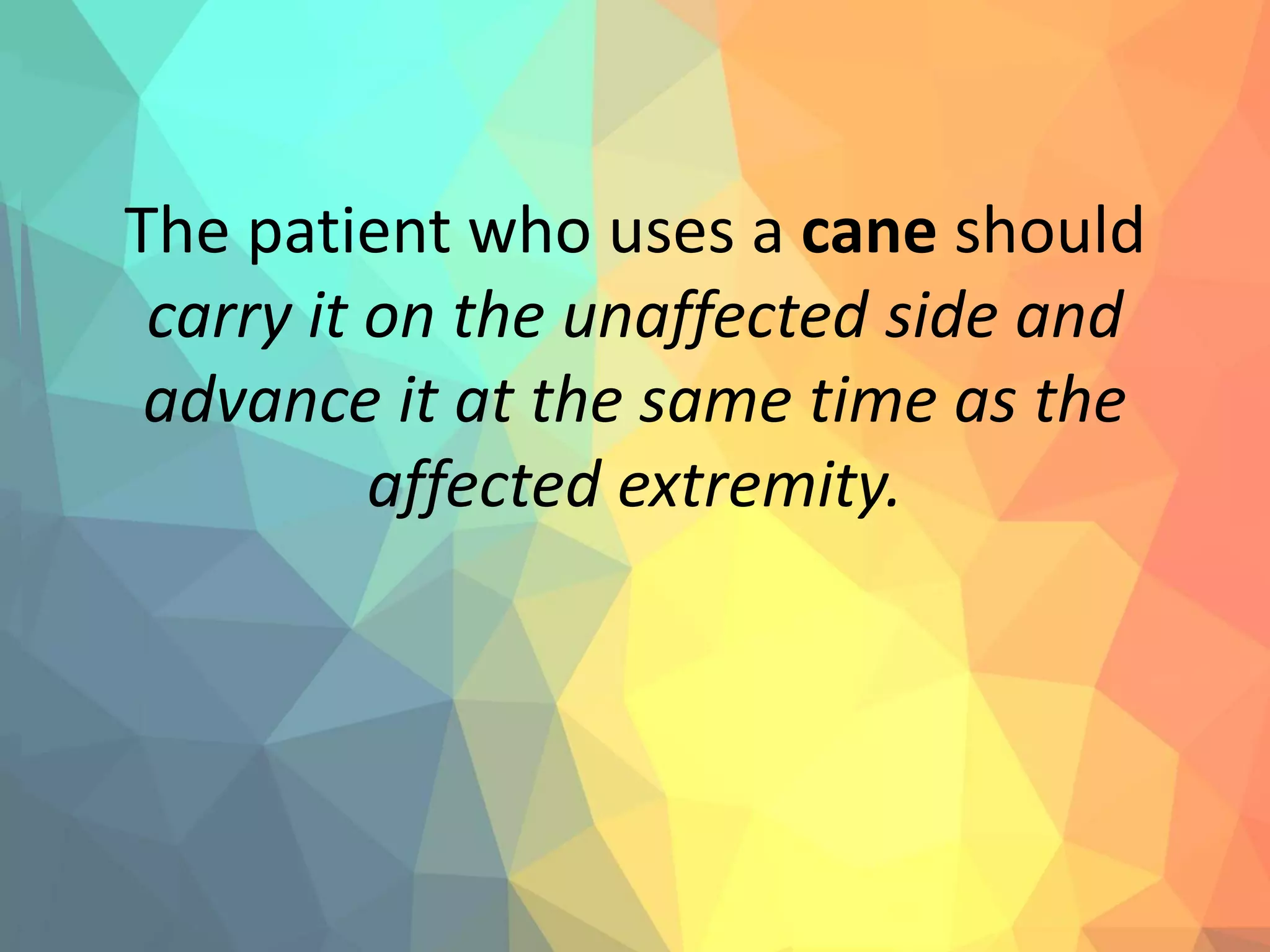
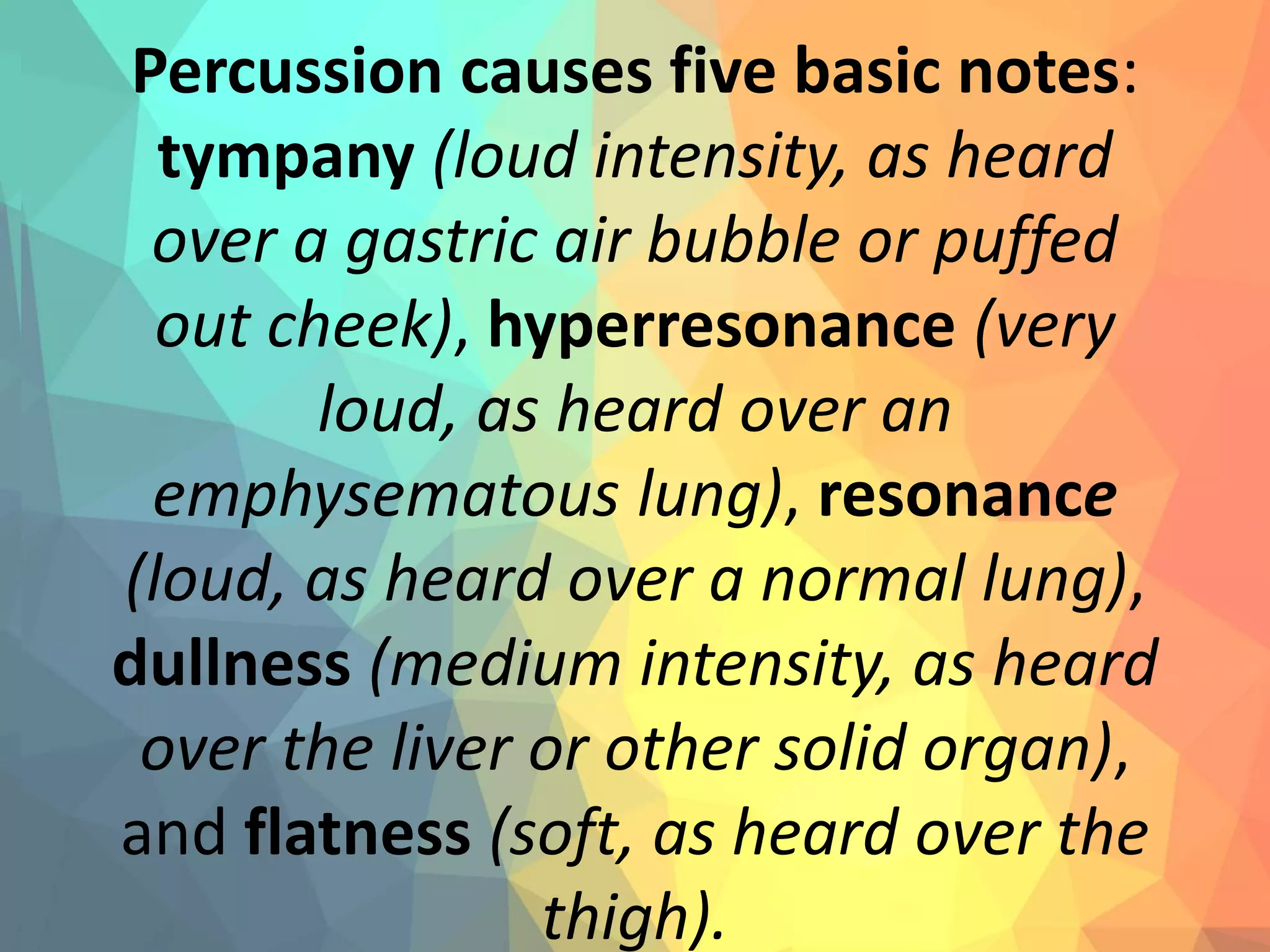
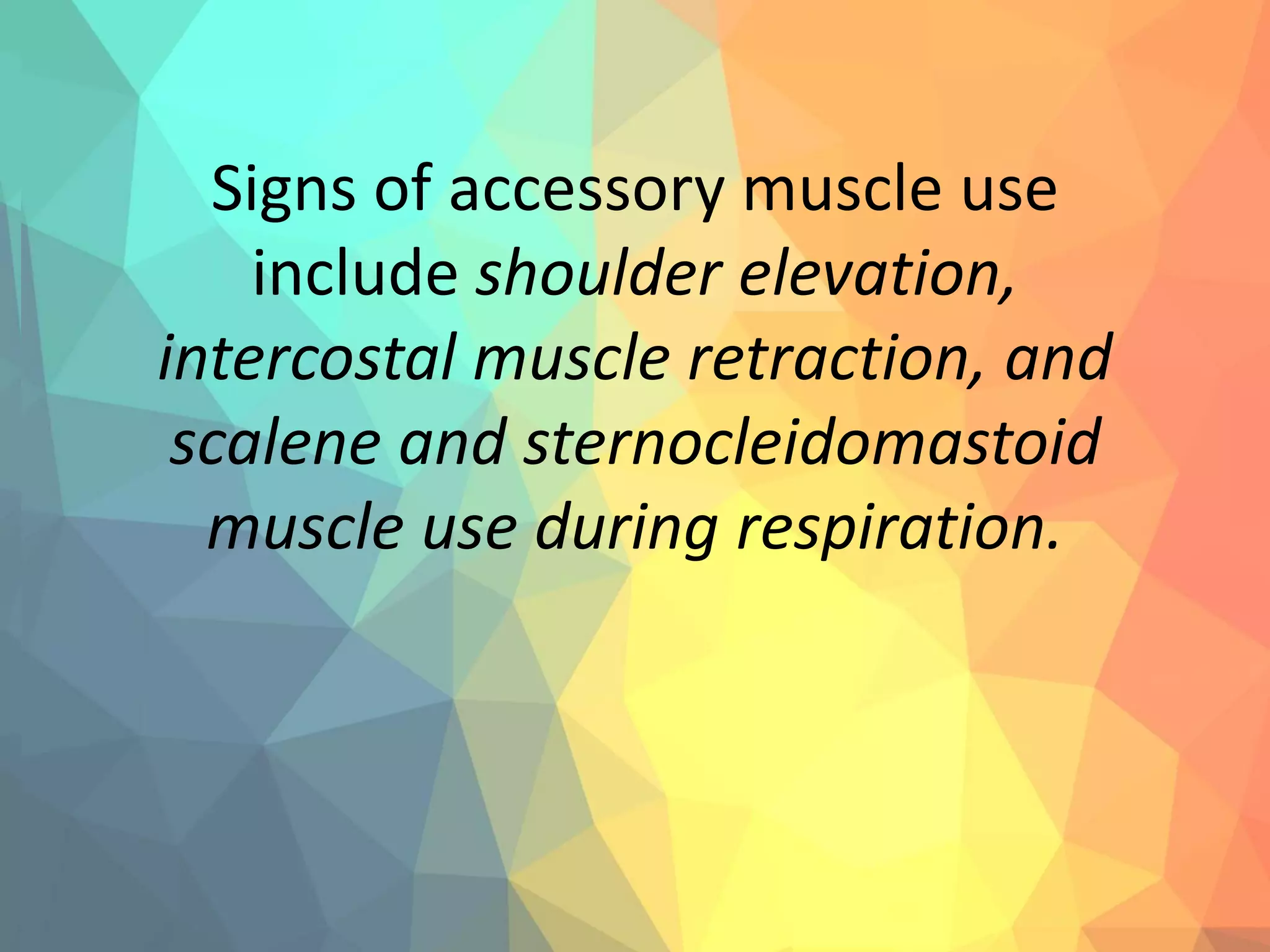
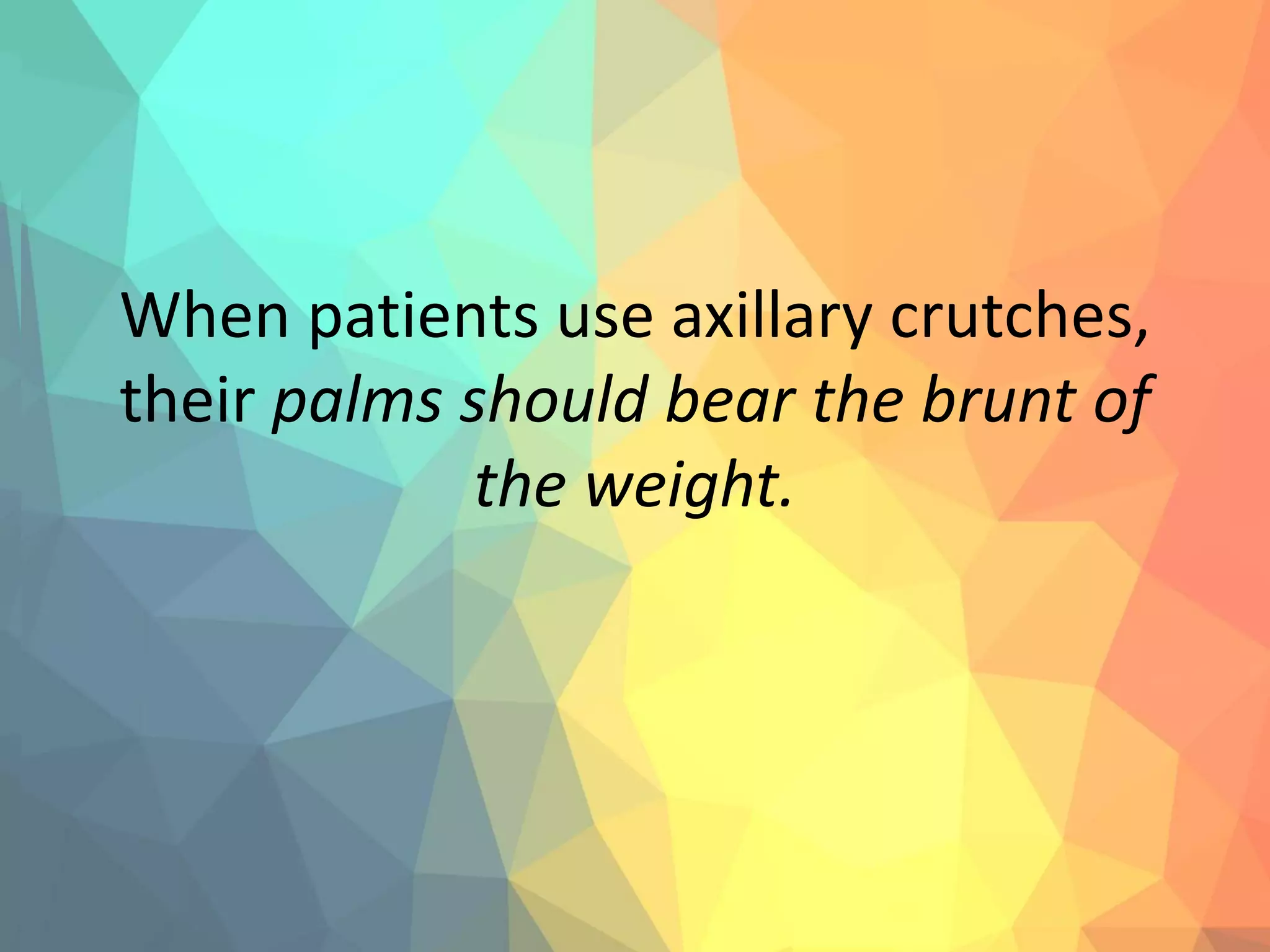
- Proper techniques for various nursing procedures such as medication administration, wound care, and patient monitoring.
- Key aspects of the nurse-patient relationship including informed consent, privacy, and safety.