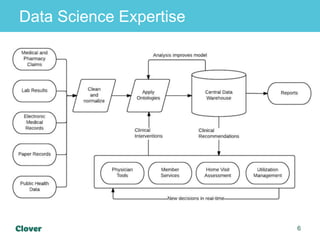
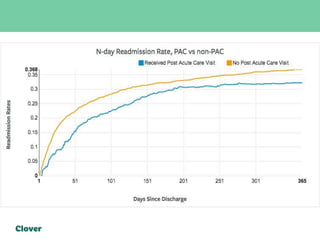
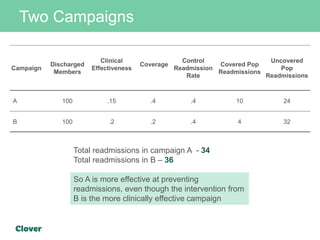
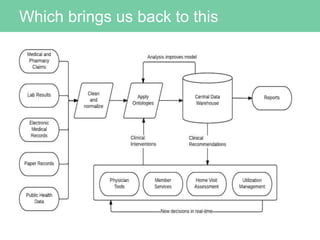
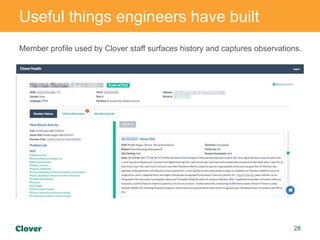
Clover Health is a technology-driven health insurance company focused on improving healthcare outcomes through data science and analytics. They aim to optimize clinical processes, manage chronic disease, and streamline operations using an in-house data warehouse and modern web development tools. Challenges faced include integrating diverse data sources, ensuring data accuracy, and maintaining efficient operations while automating processes.