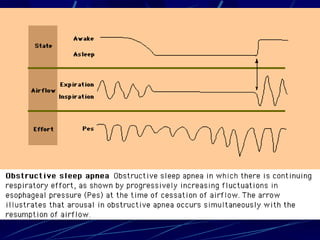
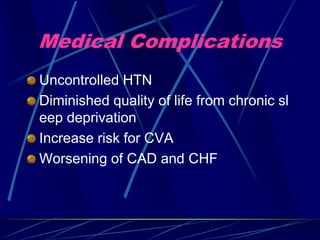
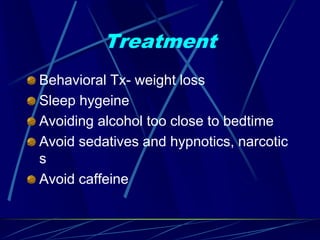
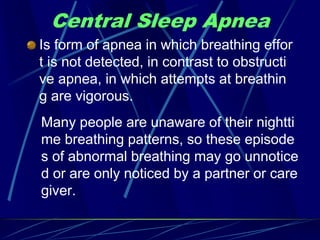
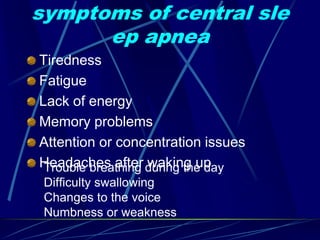
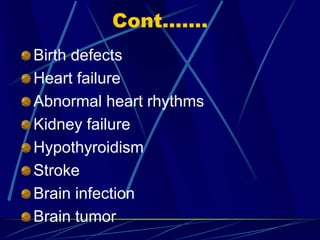
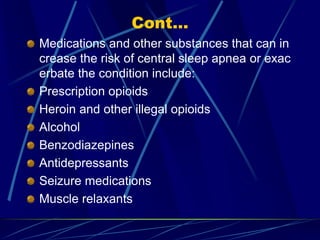
This document provides information about breathing related sleep disorders including definitions, symptoms, risk factors, diagnosis, and treatment. It discusses obstructive sleep apnea (OSA), central sleep apnea, and hypoventilation sleep apnea. OSA is characterized by partial or complete collapse of the upper airways during sleep causing breathing pauses. Central sleep apnea involves a lack of breathing effort. Hypoventilation refers to insufficient breathing during sleep leading to high carbon dioxide levels. Diagnosis involves sleep studies and treatment depends on the underlying cause but may include positive airway pressure therapy or supplemental oxygen.