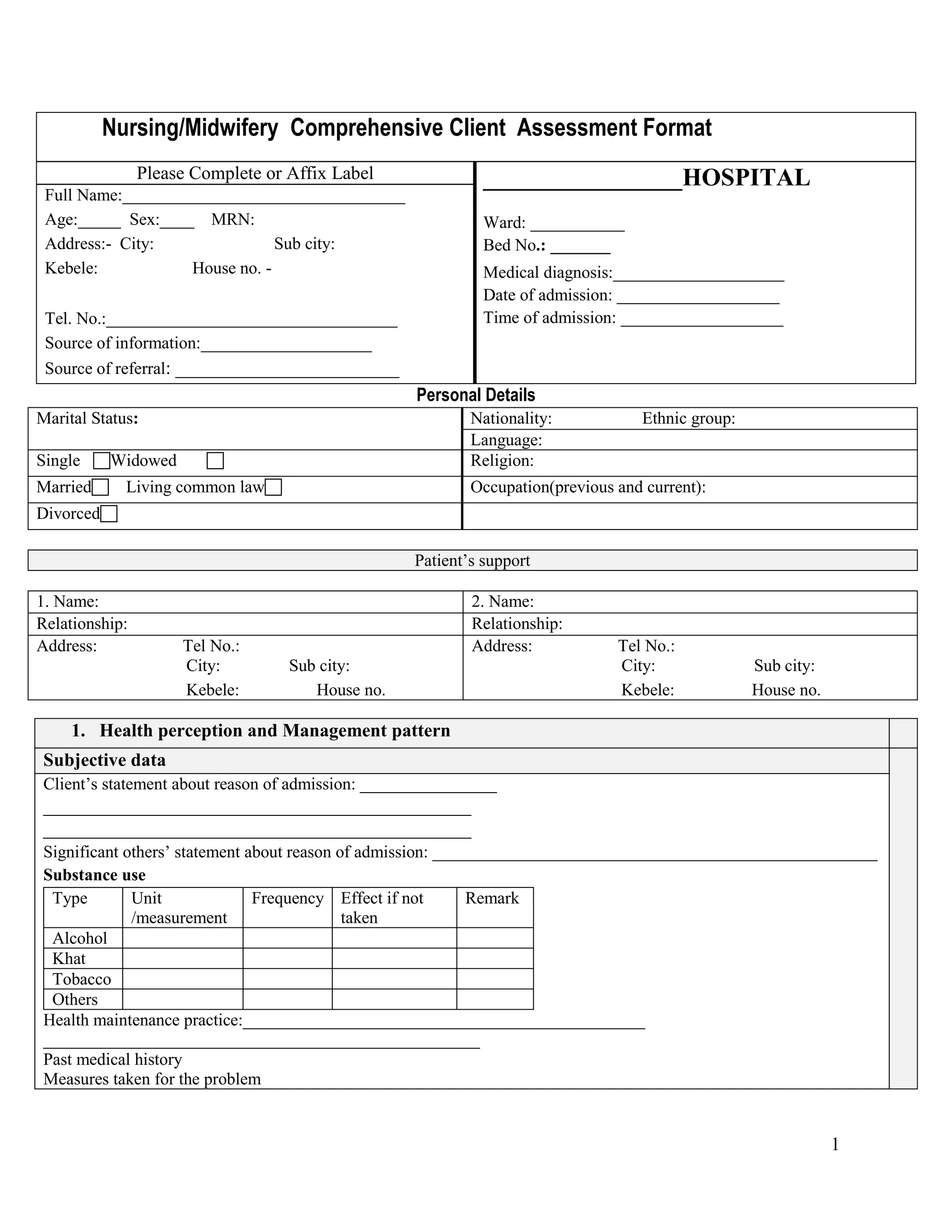
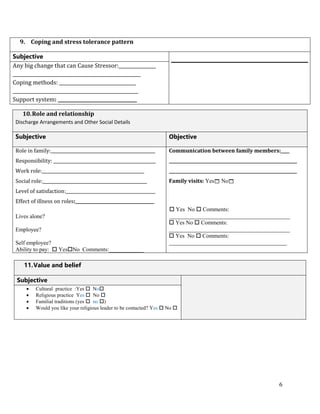
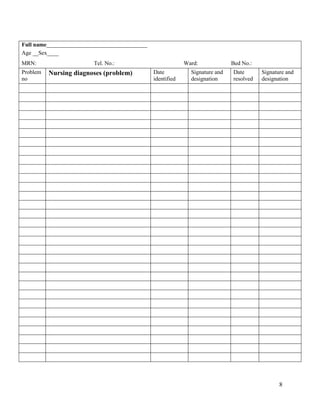
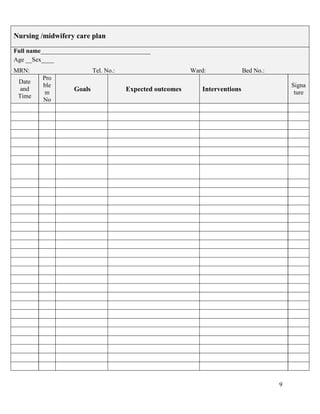
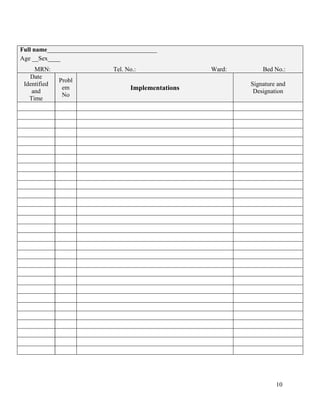
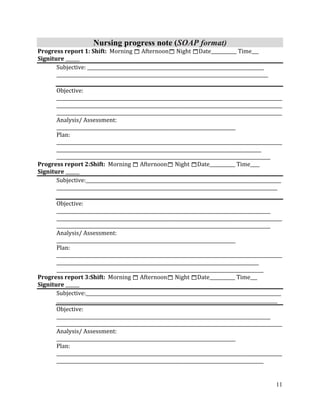
The document provides a comprehensive client assessment format used by nurses and midwives. It collects personal details, health history, physical assessment findings, and social information across 12 sections, including the client's personal and medical history, nutrition, elimination, activity, rest, sexuality, cognitive function, self-perception, coping, roles, values and discharge planning. The assessment is used to identify nursing diagnoses, develop a care plan with goals and interventions, and document progress over time using a subjective, objective, assessment, plan (SOAP) format.