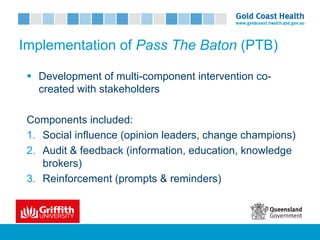
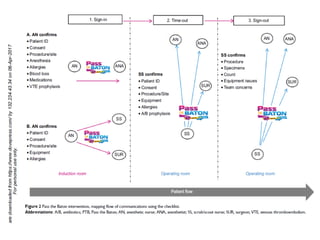
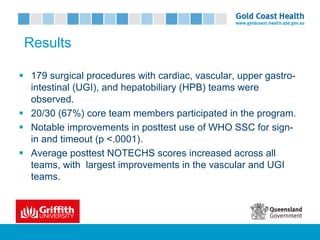
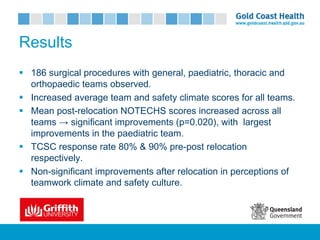
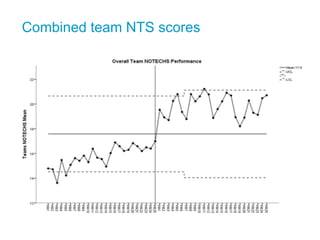
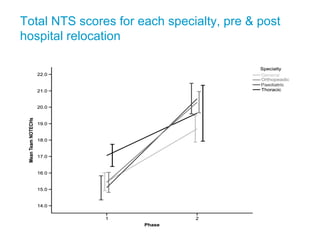
This document summarizes three case studies conducted by Dr. Brigid Gillespie and her research team examining ways to improve team performance and safety culture in surgical settings. The first case study evaluated a brief team training program and found improvements in non-technical skills and checklist adherence. The second studied changes following a hospital relocation and found increased team performance scores. The third evaluated an intervention called "Pass the Baton" that improved checklist use, teamwork climate, and safety culture through multi-component implementation strategies. The studies demonstrate the impact of training, environmental factors, and tailored implementation approaches on surgical team outcomes.


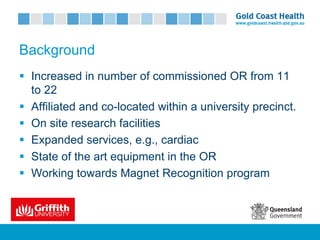

![Comments
§ First study to examine process changes in surgical team
performance during such a major upheaval.
§ Results suggest a naturally occurring process change over time.
§ Environmental factors (e.g. ergonomic) may support collaborative
work.
§ Increase in staff numbers – i.e., new staff creates a positive
change in work place culture.
§ Communication & teamwork among surgical teams improved in
transient teams [Korkiakangas et al. (2016) & Gillespie et al. (2013)]](https://image.slidesharecdn.com/brigidgillespie-170720022131/85/Brigid-Gillespie-Griffith-University-18-320.jpg)