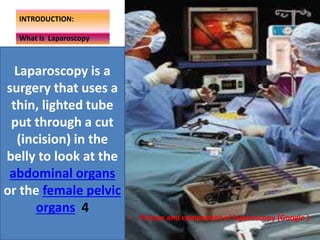
This document discusses different techniques for teaching laparoscopic surgery to surgeons and registrars in North Queensland, Australia. It provides background on the emergence of laparoscopic surgery and traditional apprenticeship-based training versus simulation-based training using virtual reality simulators. The study aims to assess the knowledge and attitudes of surgeons and registrars regarding these teaching techniques and determine if virtual reality training videos add educational value. A descriptive study using surveys and interviews of surgeons and registrars will be conducted to analyze their ratings and preferences for web-based training videos and assess their impact on surgical skills acquisition.