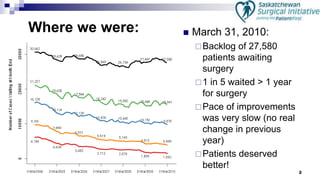
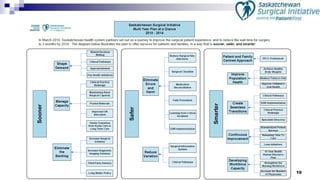
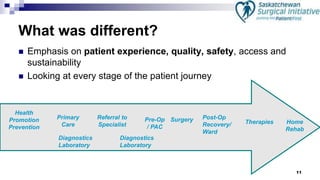
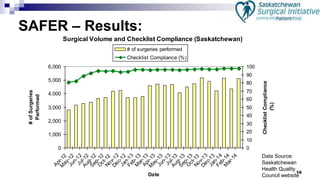
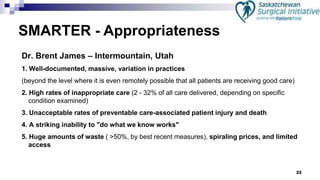
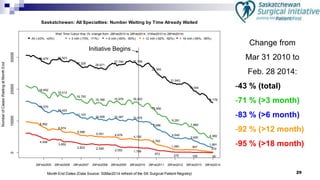
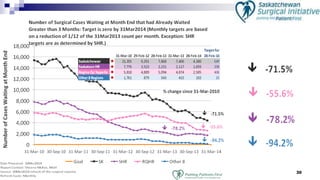
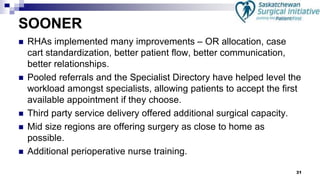
The Saskatchewan Surgical Initiative aimed to transform the surgical patient experience by reducing wait times and improving safety and quality. With a focus on patient involvement, comprehensive planning, and continuous improvement, the initiative successfully decreased the backlog of surgery patients and established a system-wide culture shift towards patient-centered care. Key lessons included the importance of leadership, meaningful patient representation, and engaging physicians in improvement efforts.