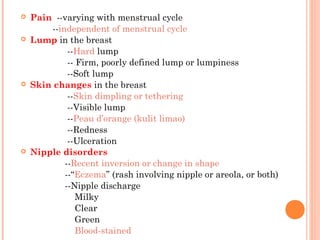
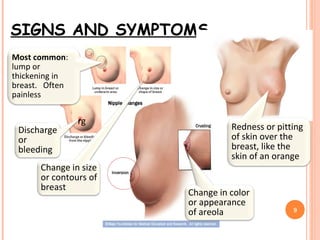
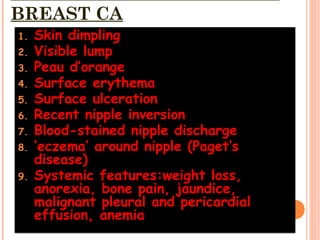
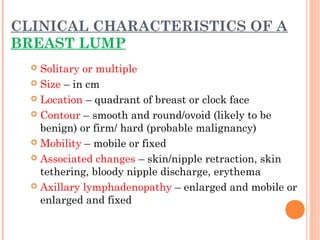
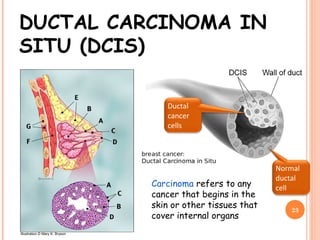
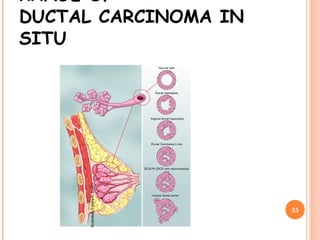
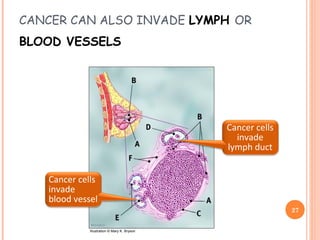
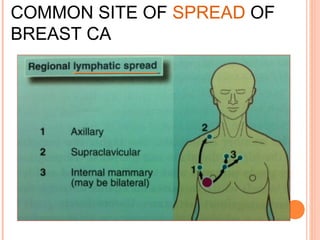
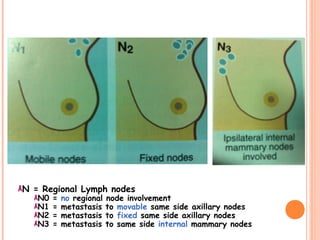
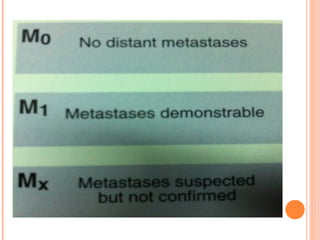
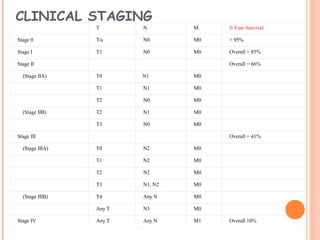
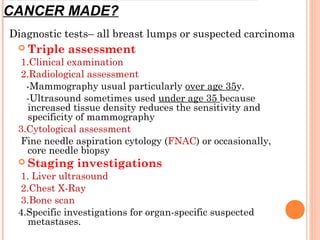
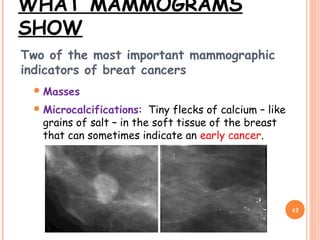
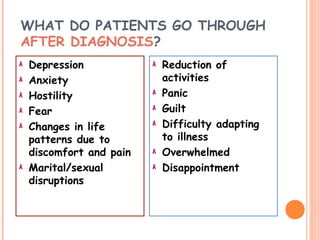
This document provides information on techniques for breast examination and diagnosis and treatment of breast cancer. It discusses signs and symptoms of breast cancer including lumps, skin changes, and nipple disorders. It describes ductal carcinoma in situ and invasive ductal carcinoma as well as stages of breast cancer. Detection methods like mammography and treatments including surgery, chemotherapy, radiation, and prevention strategies are summarized.