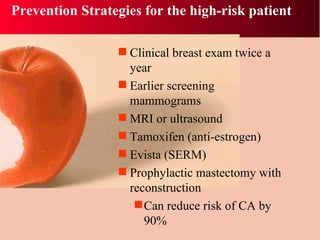
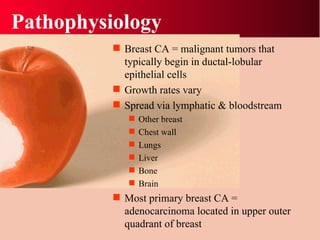
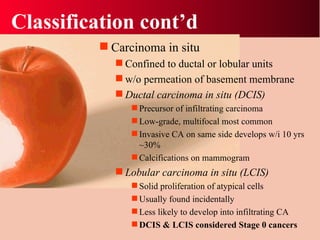
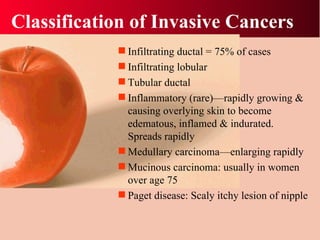
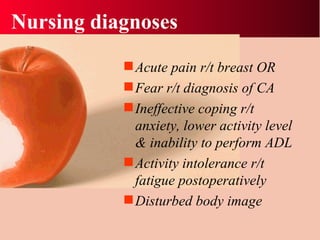
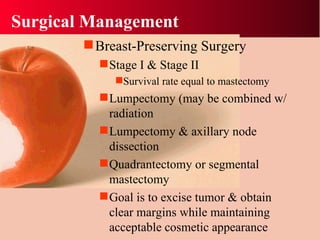
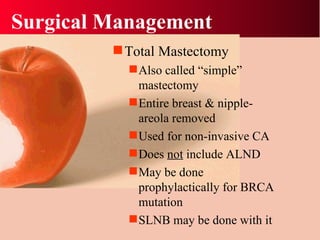
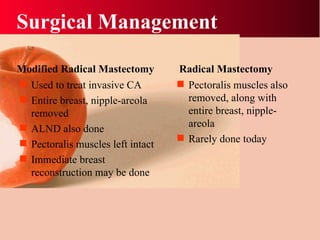
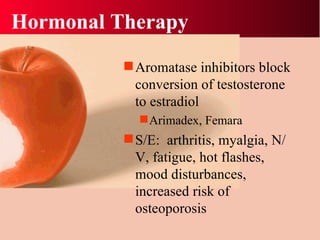
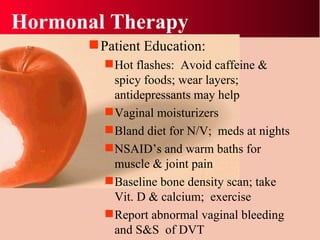
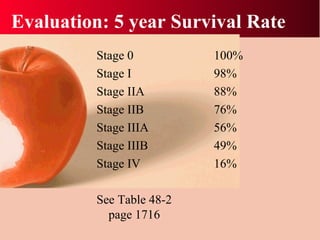
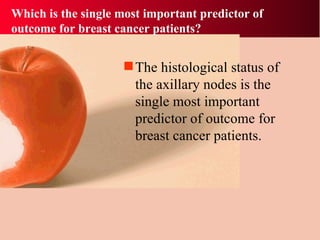
Breast cancer is the most common cancer in women, affecting about 1 in 8 women over their lifetime. Risk factors include age, family history, certain genetic mutations, reproductive history, obesity, and alcohol use. Screening mammography can detect breast cancer early when treatment is most effective. Treatment may involve surgery such as lumpectomy or mastectomy, radiation, chemotherapy, hormone therapy, and breast reconstruction. Side effects of treatment can include pain, lymphedema, fatigue, and changes in body image. Long term follow up focuses on monitoring for recurrence and managing side effects.