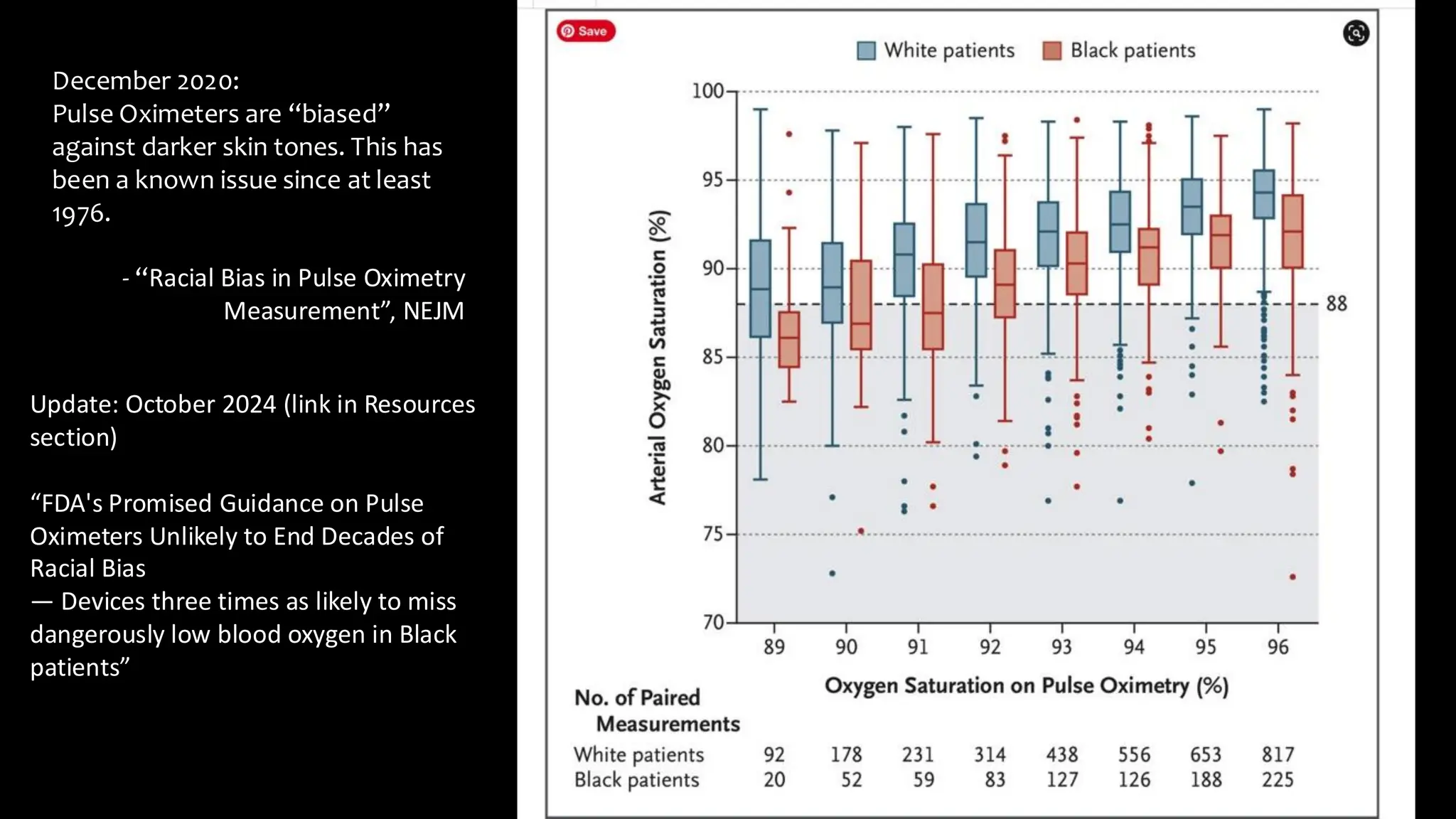
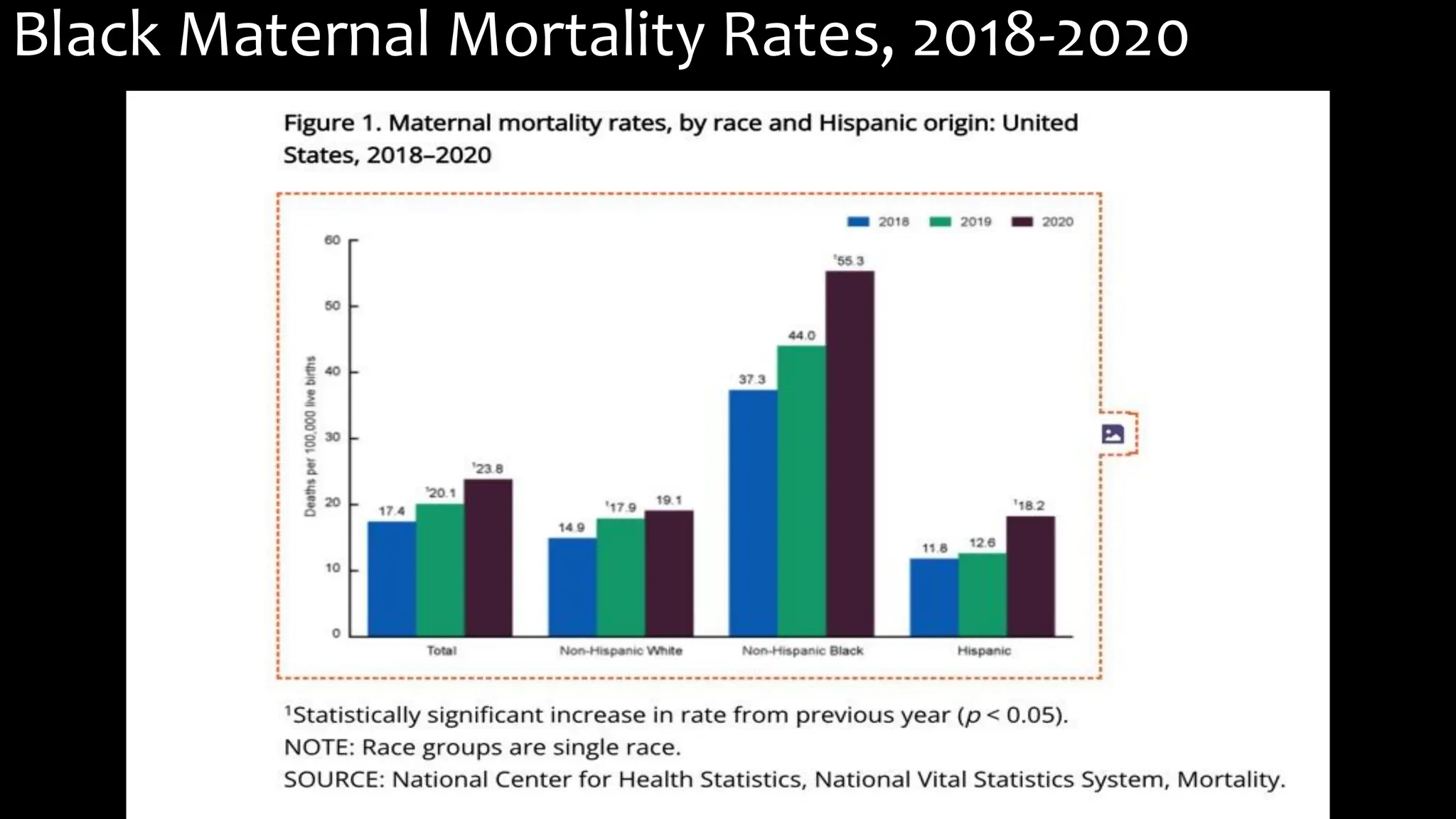
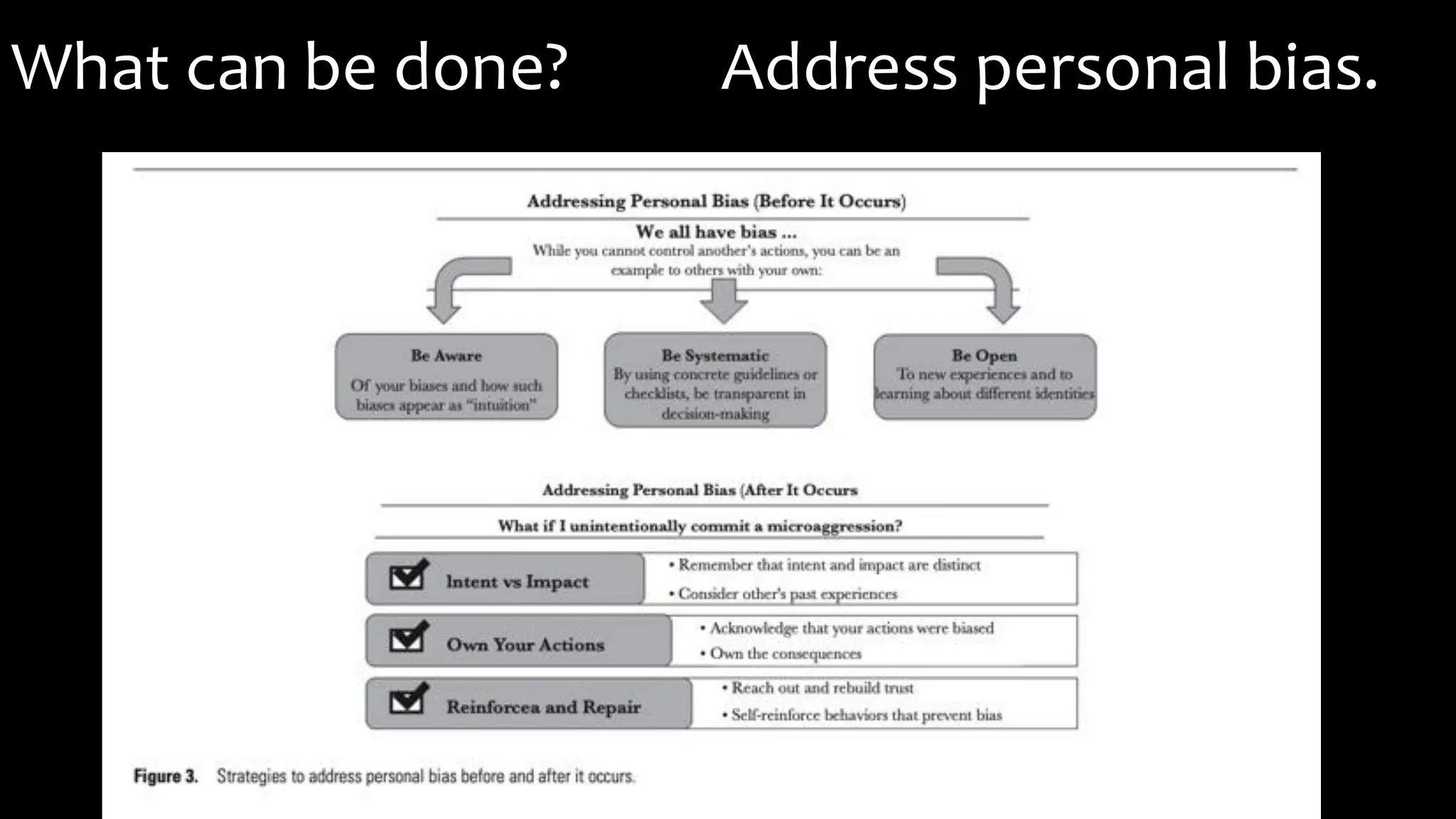
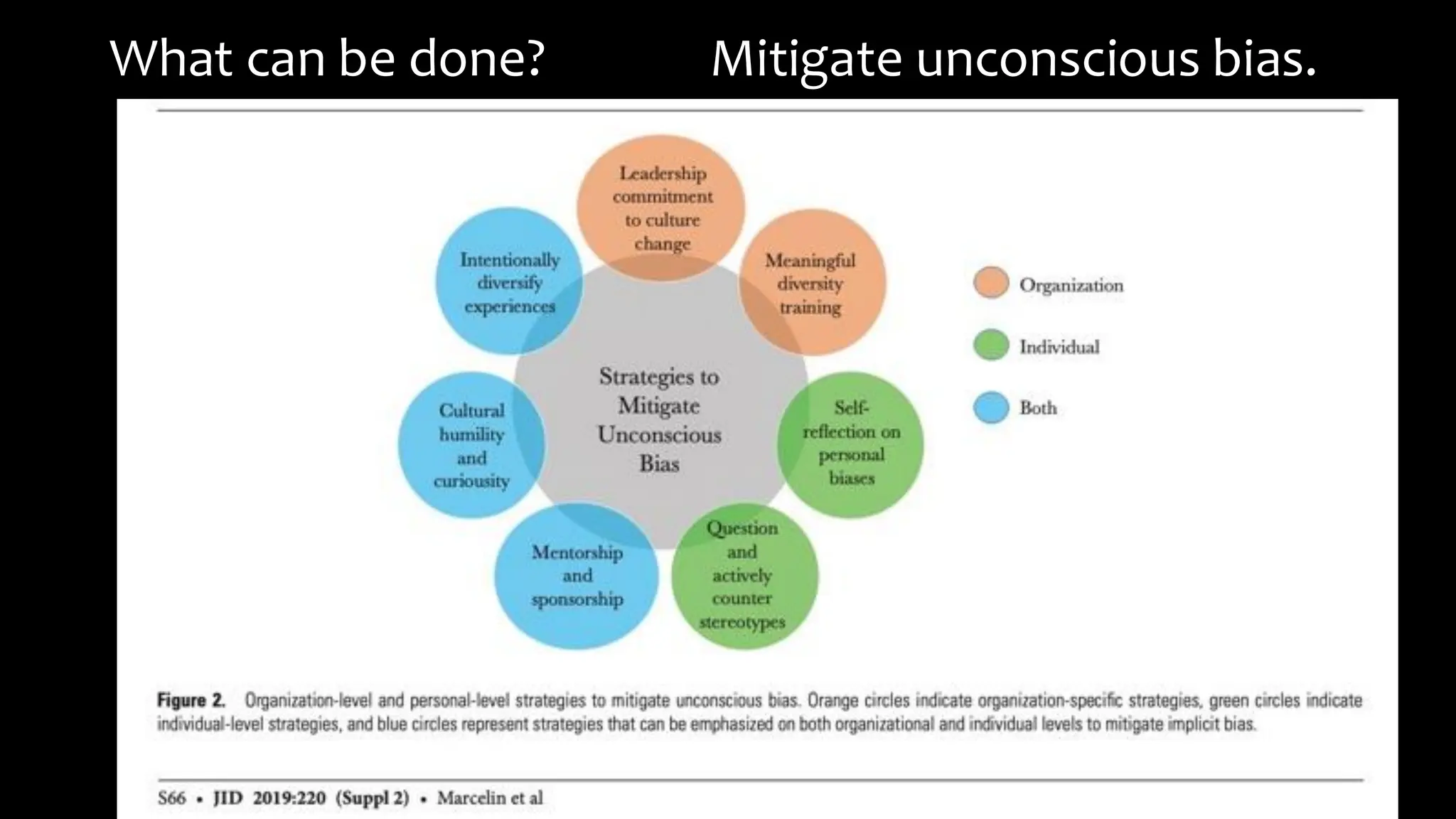
The document provides an evidence-based overview of bias in healthcare, emphasizing the impact of both conscious and unconscious biases on patient care and health outcomes, particularly for marginalized groups. It discusses various types of biases, including racial and weight biases, their systemic roots in structural racism, and their effects on health disparities and inequities. Additionally, it outlines strategies for addressing bias within healthcare systems, including training and policies aimed at promoting health equity.