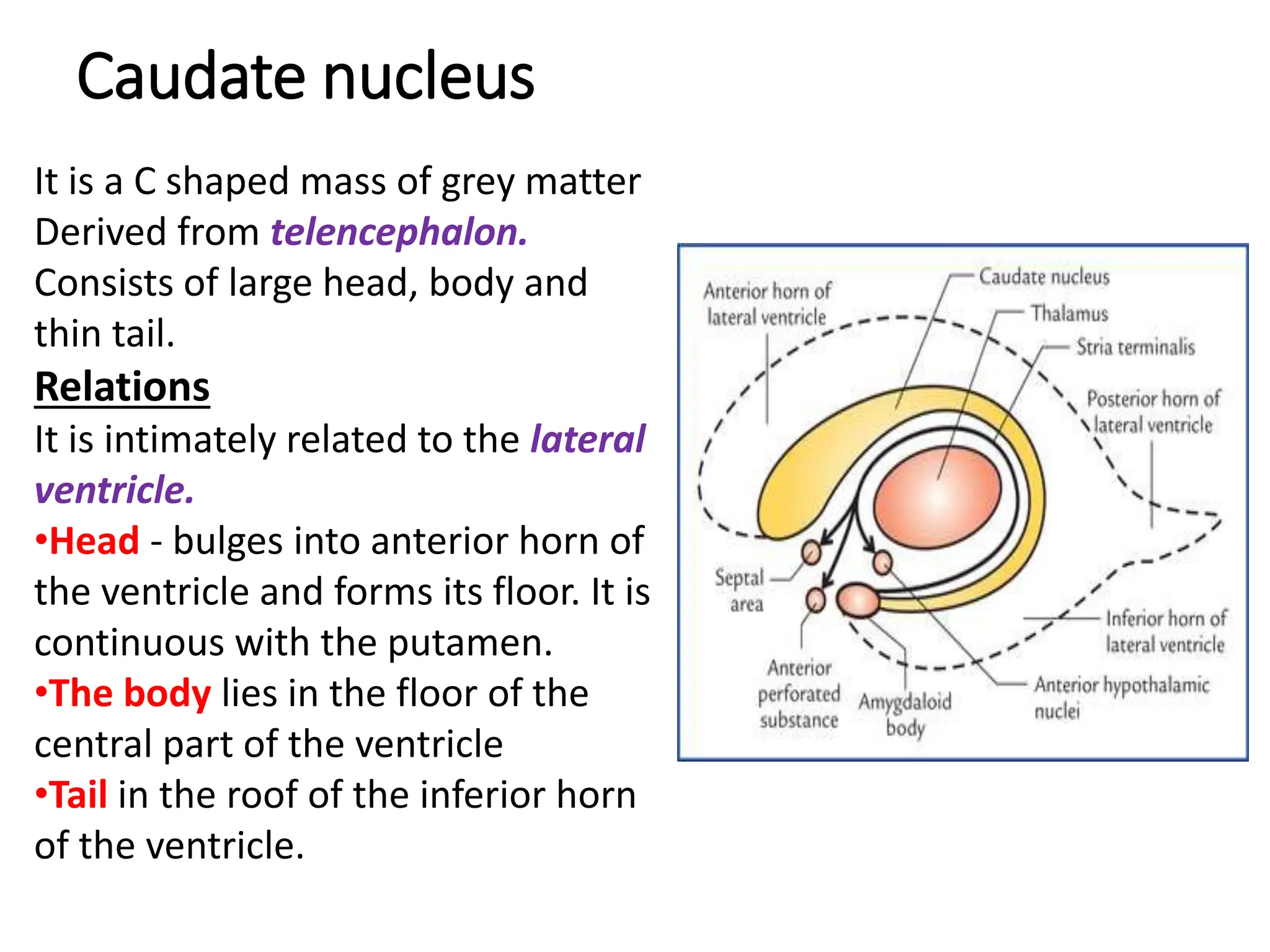
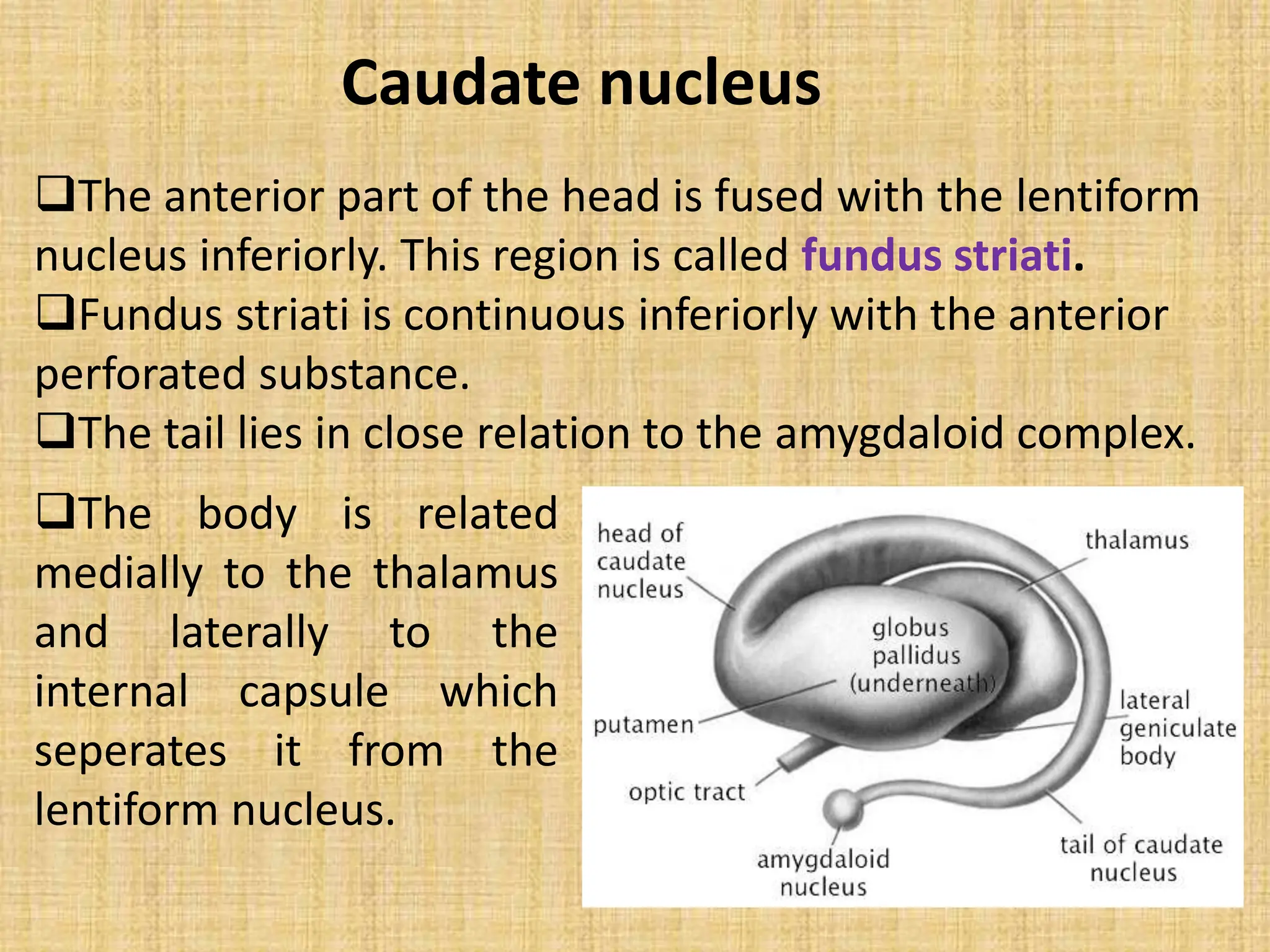
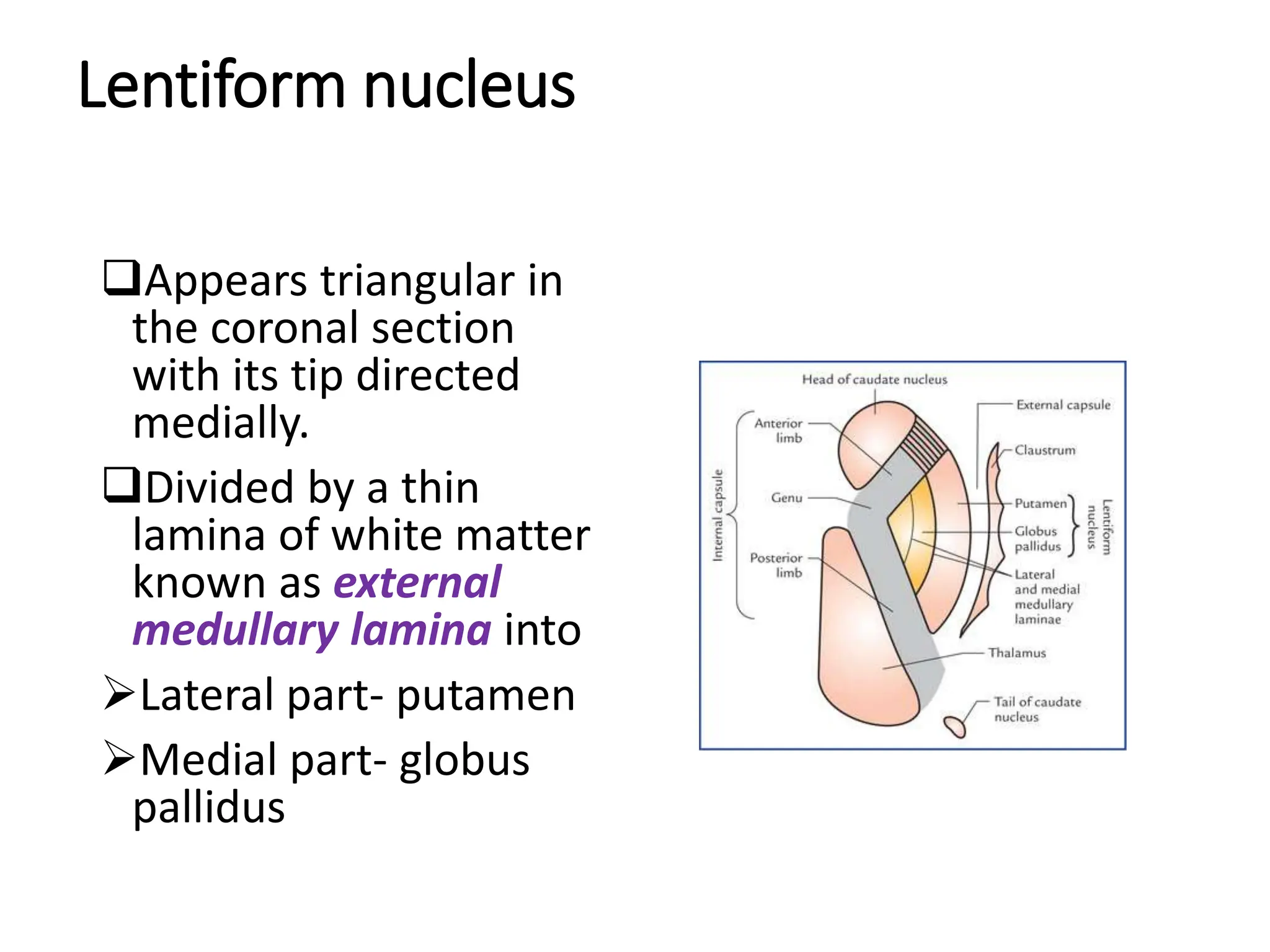
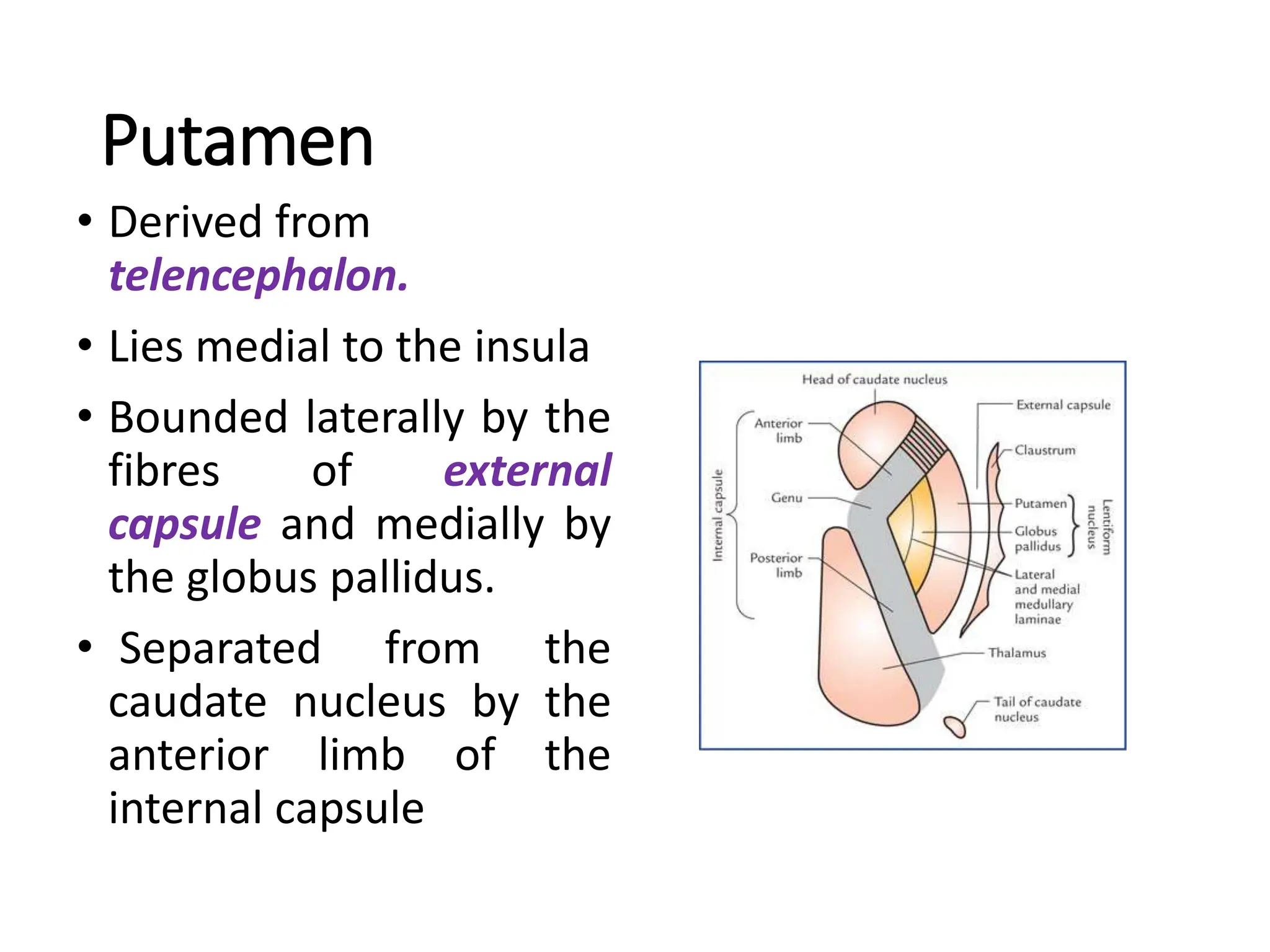
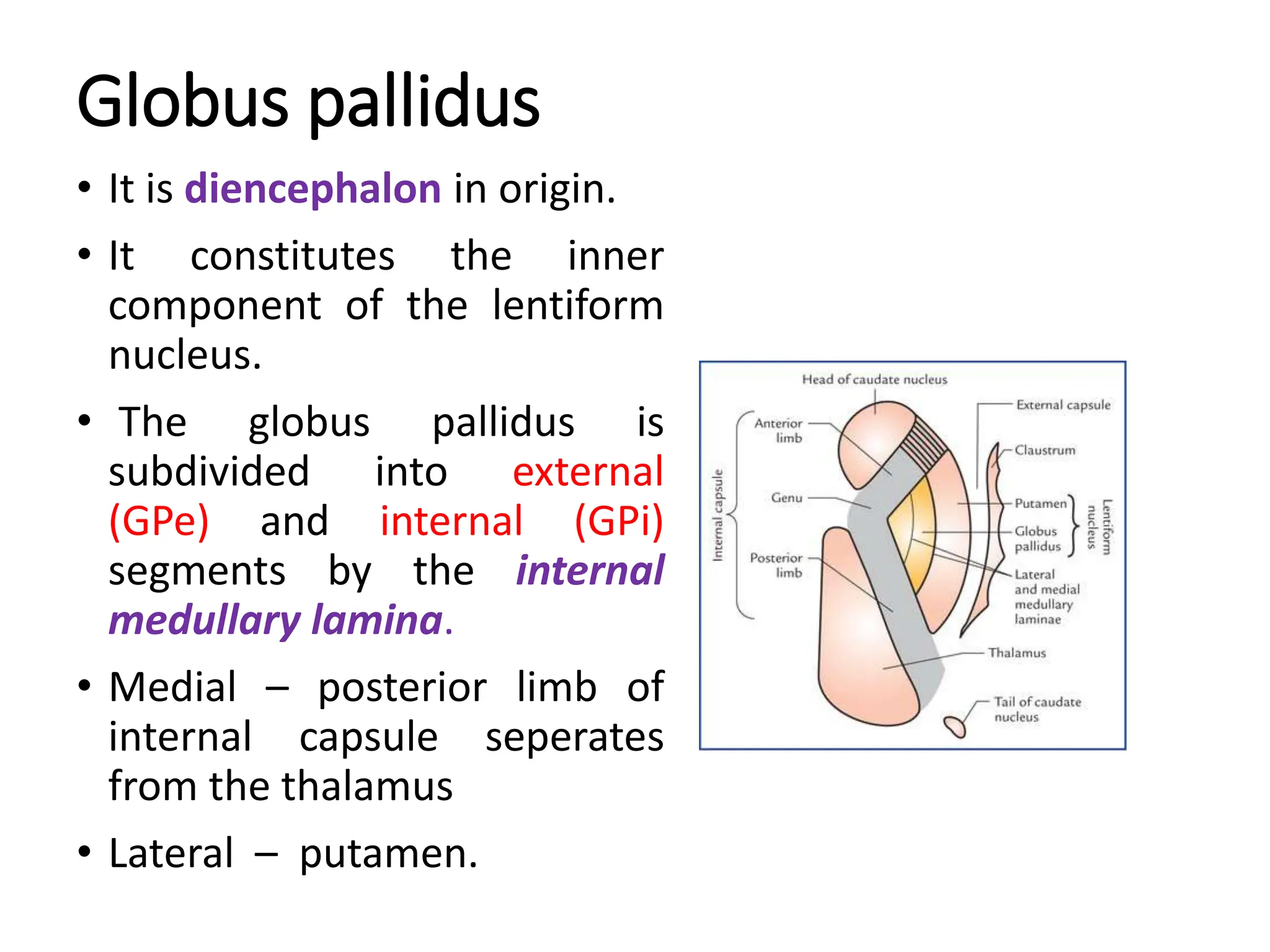
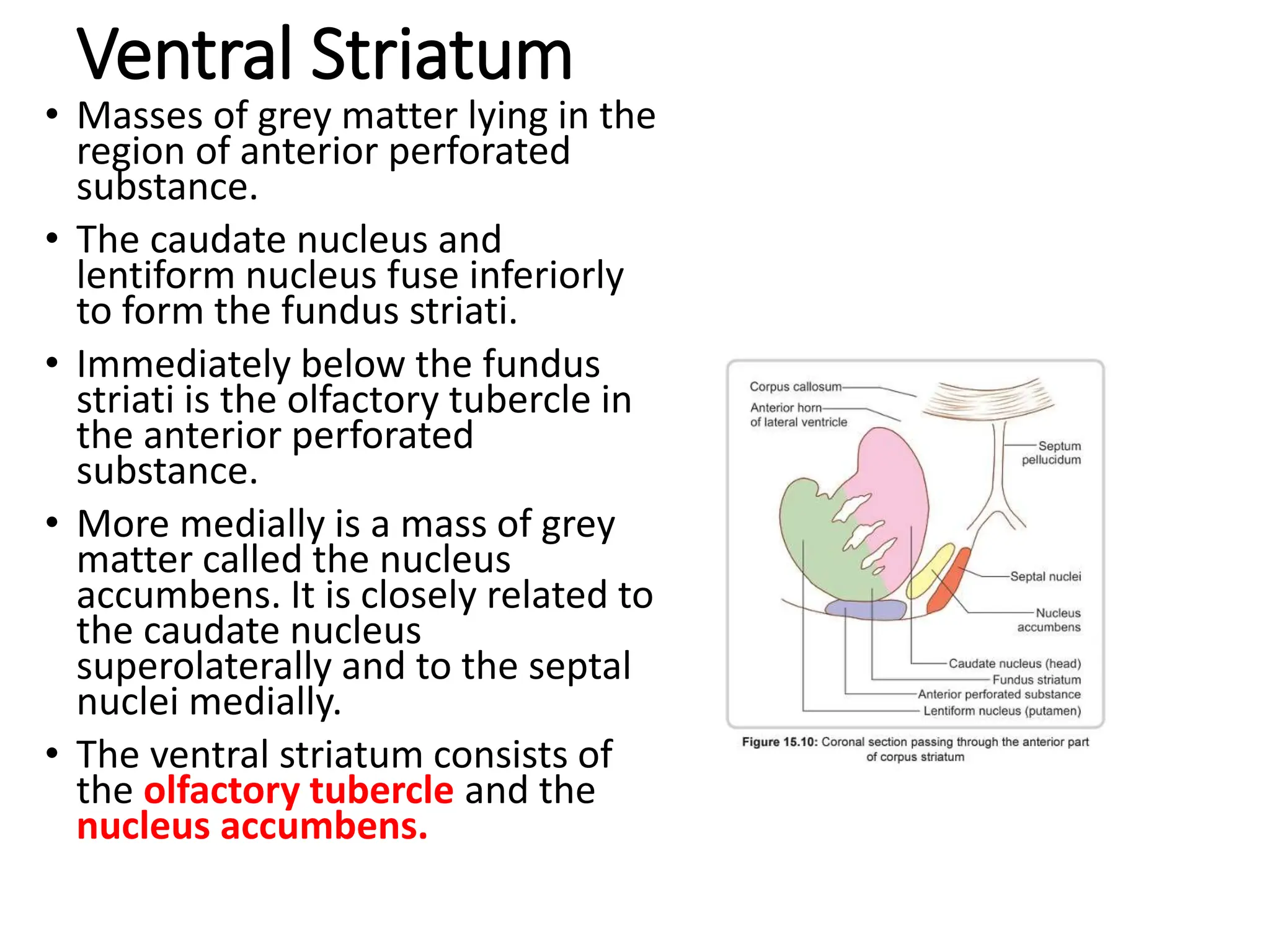
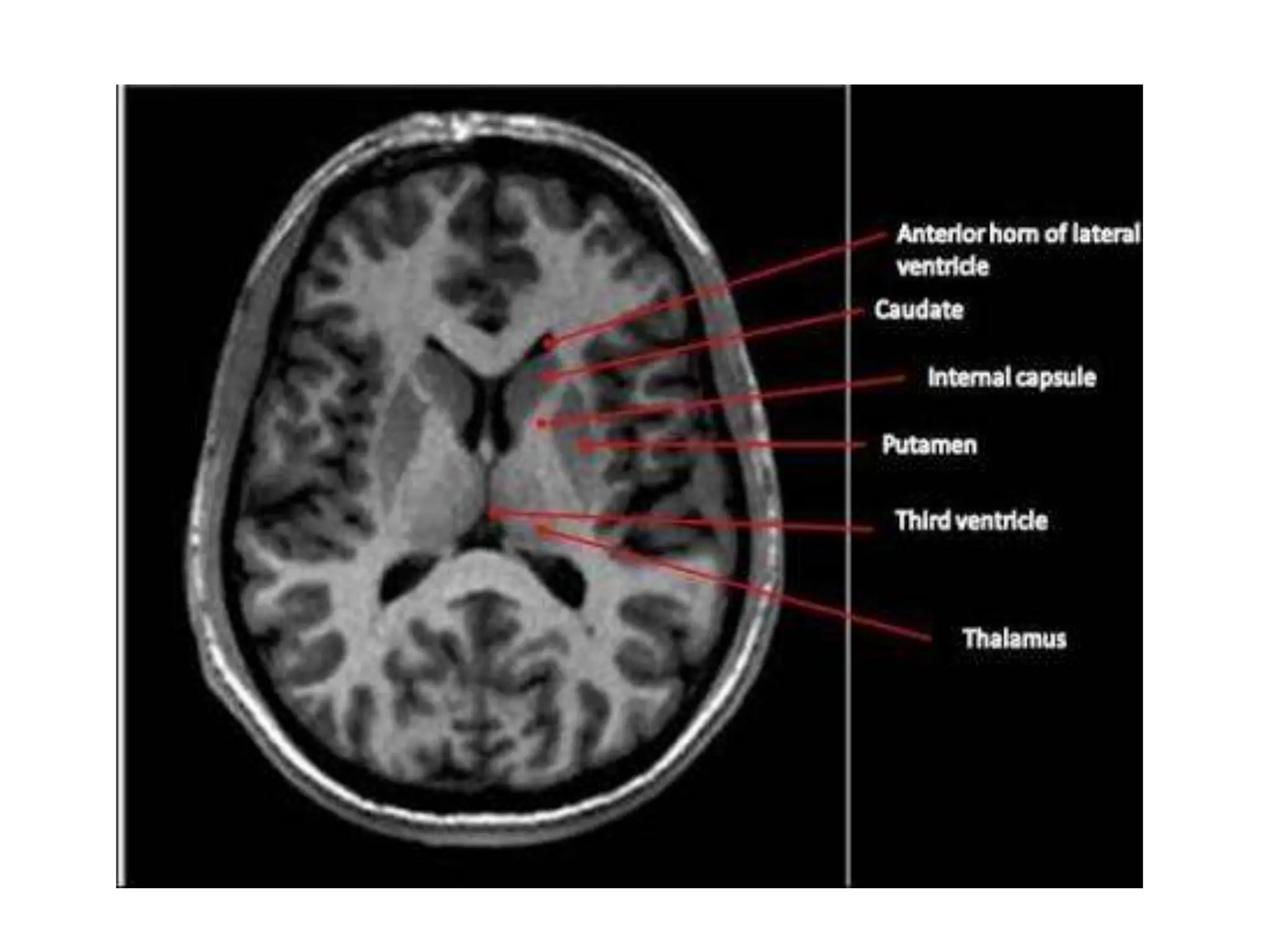
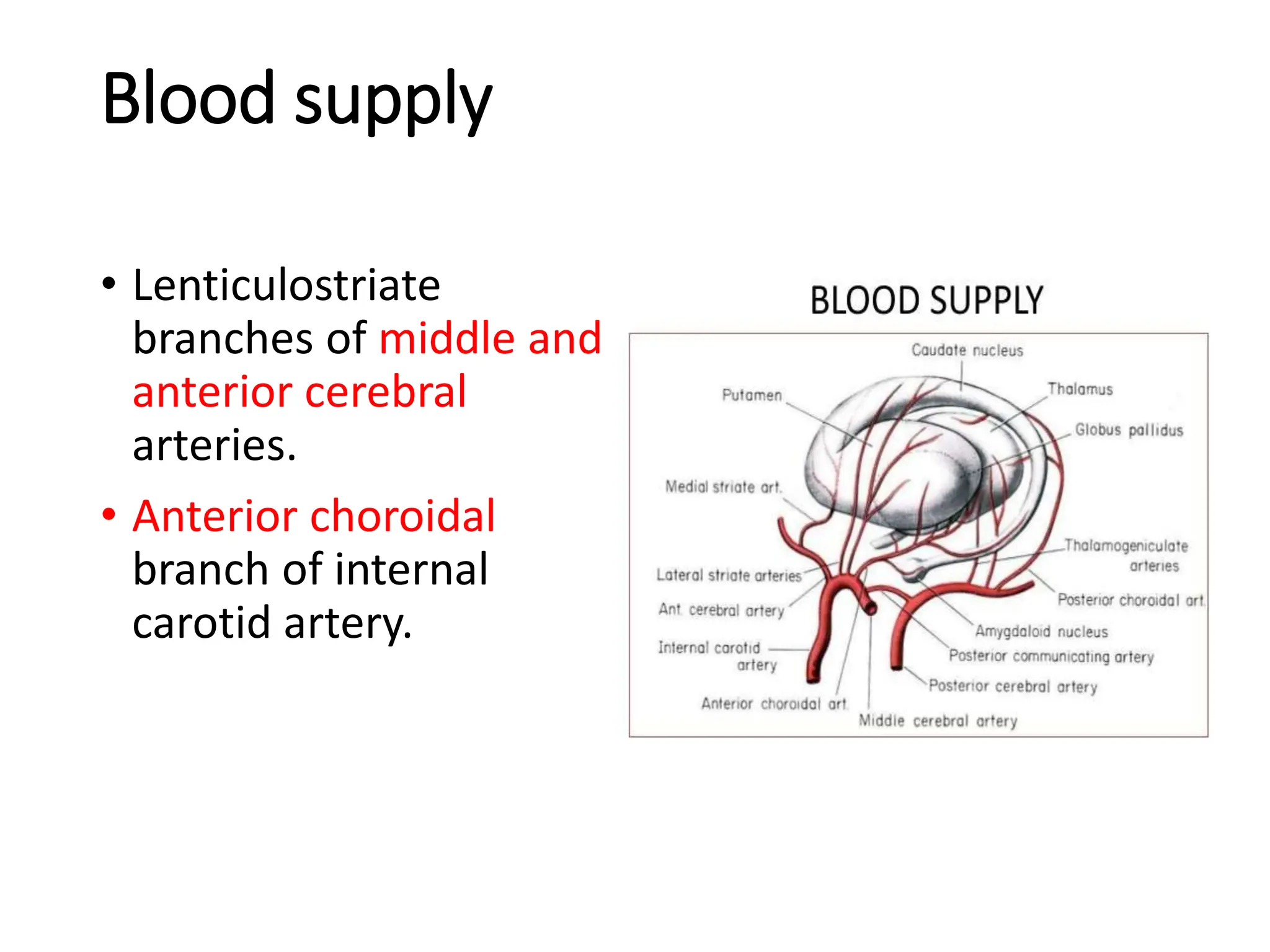
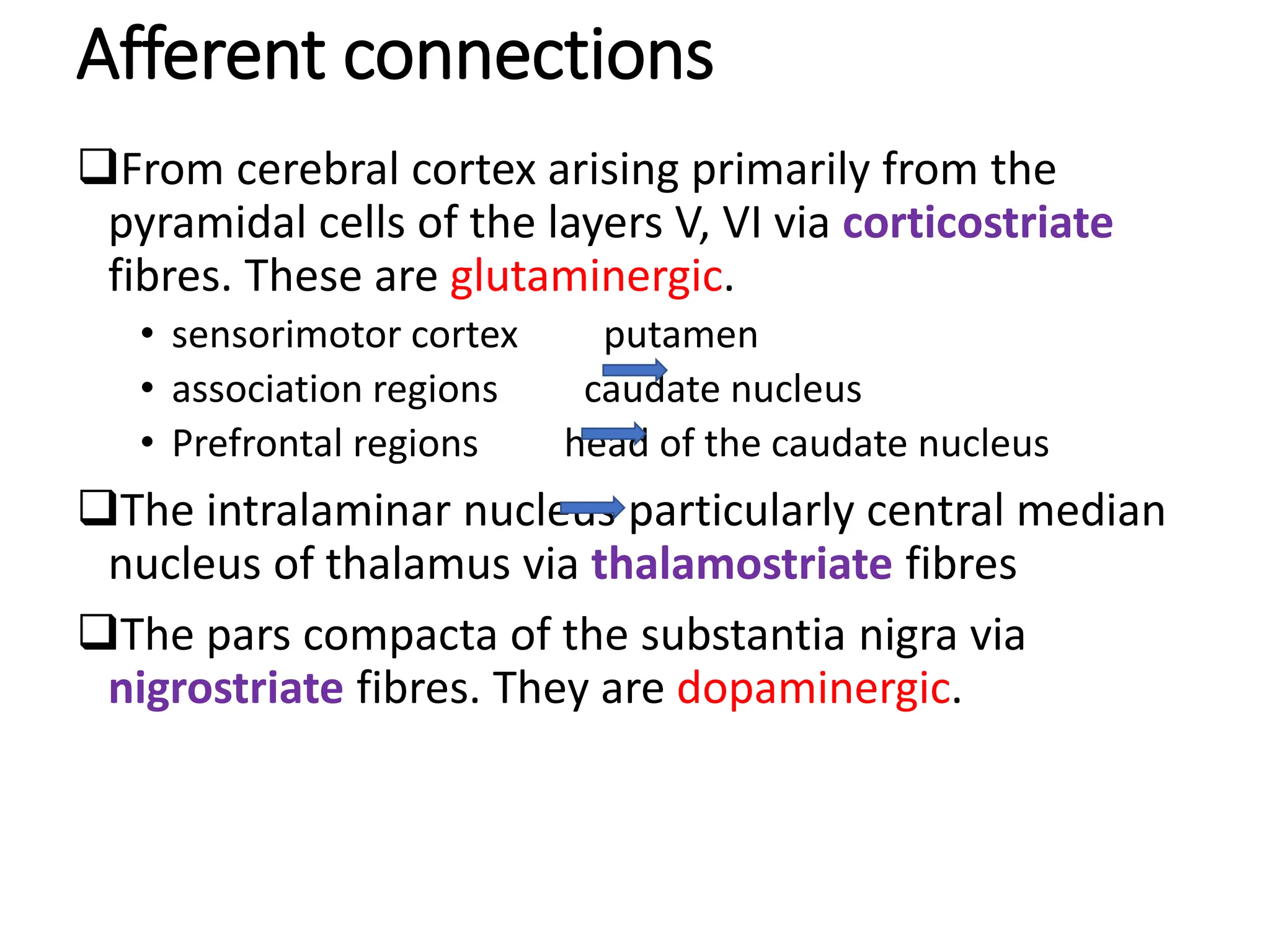
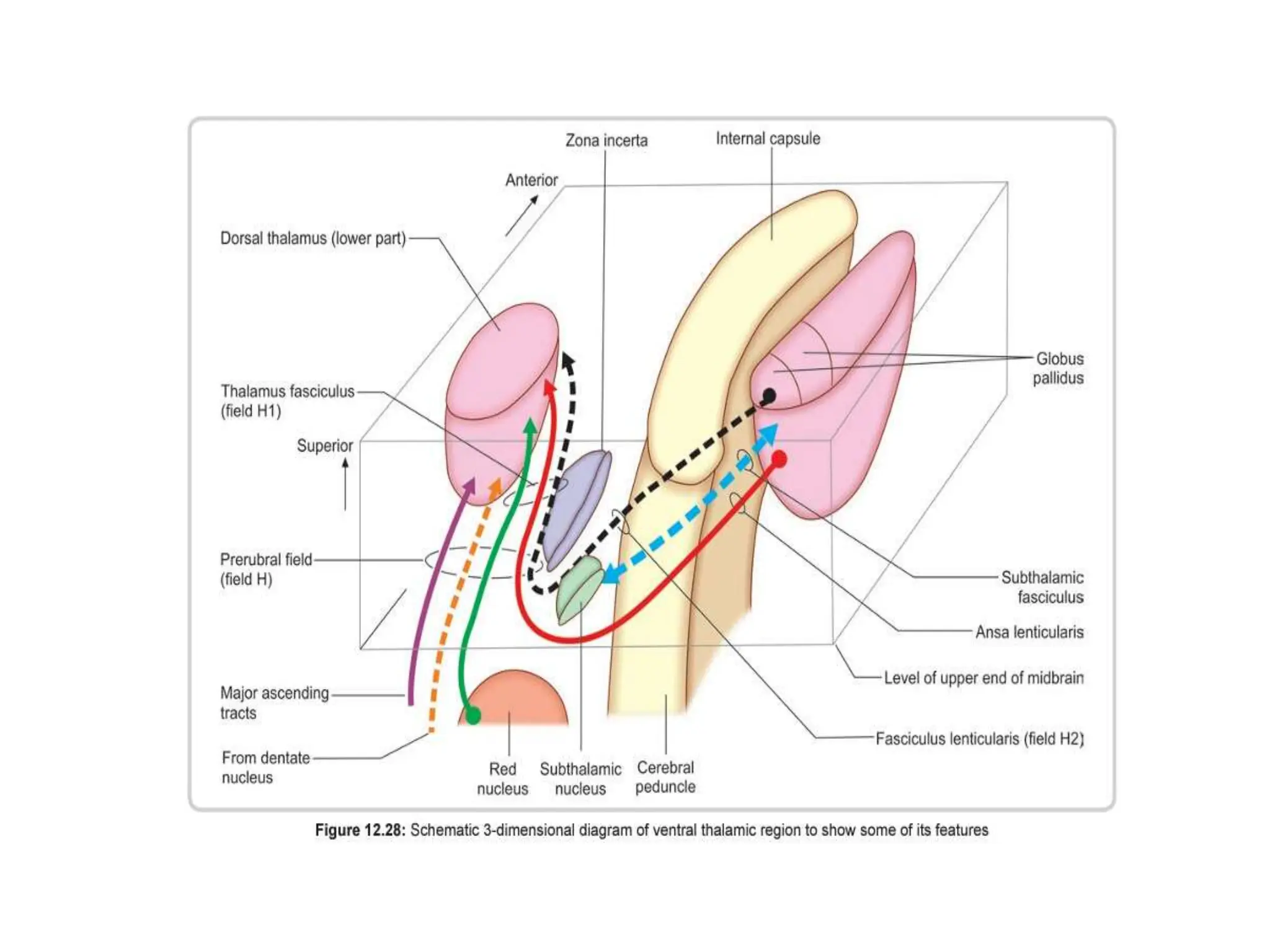
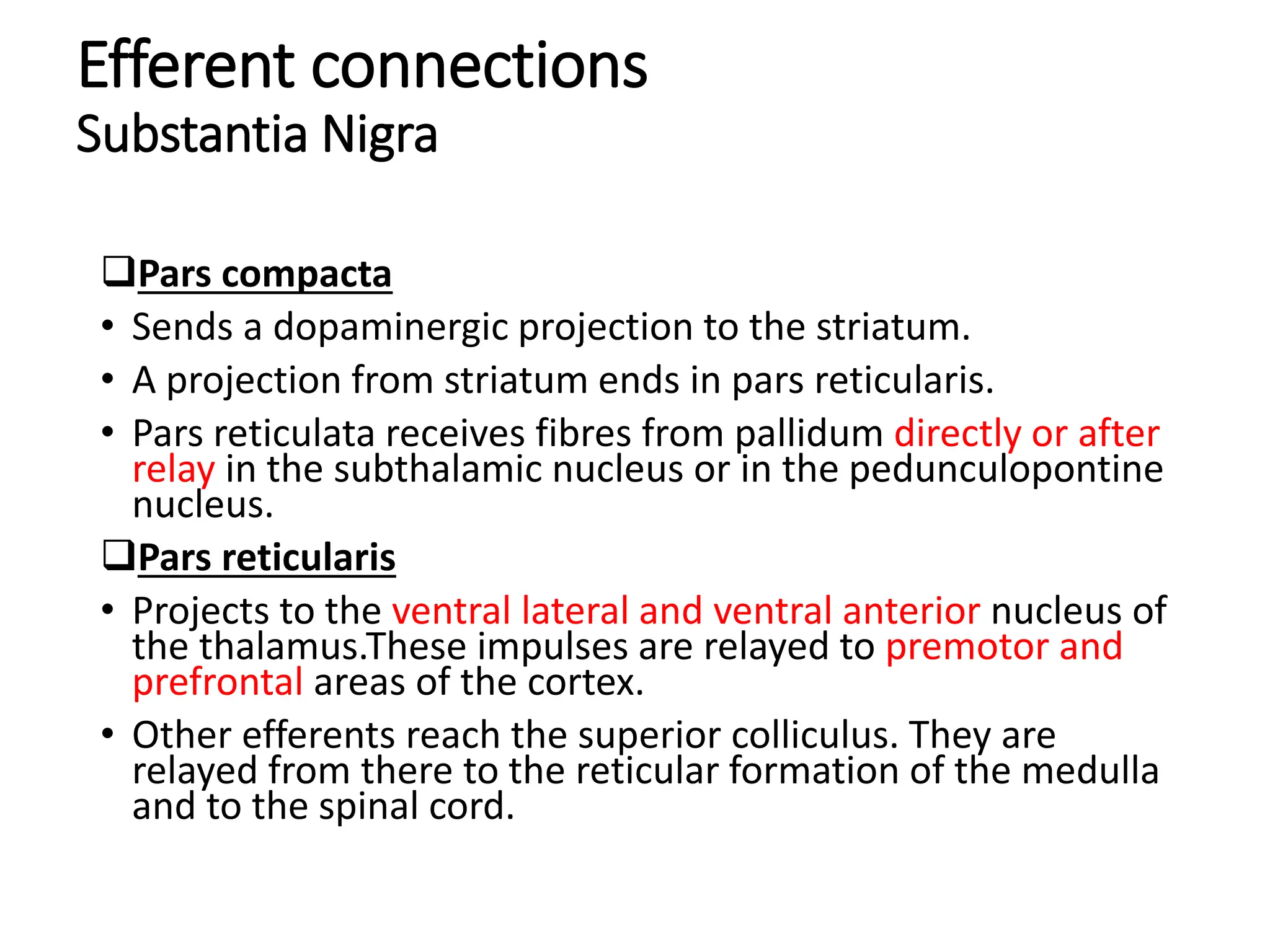
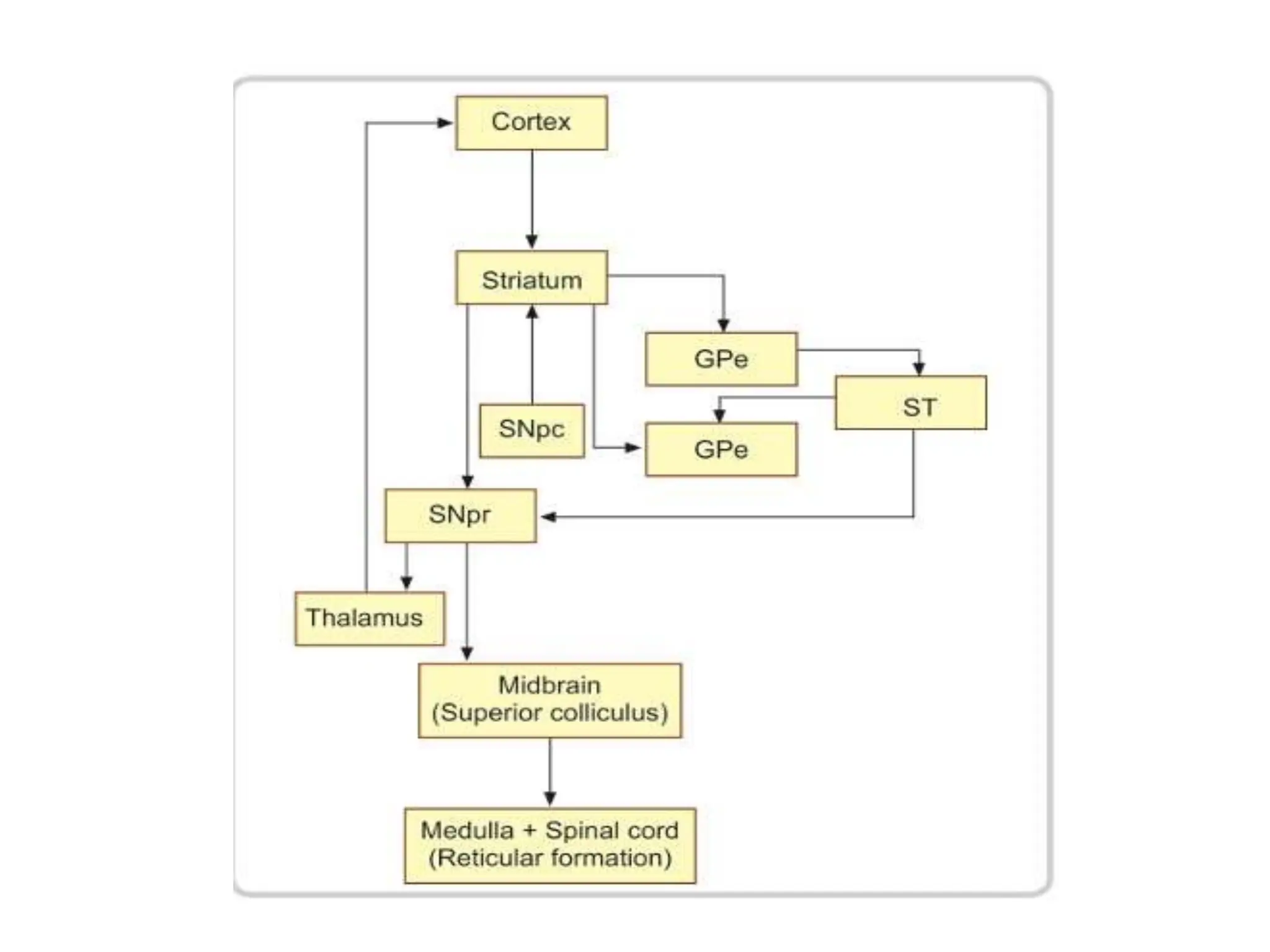
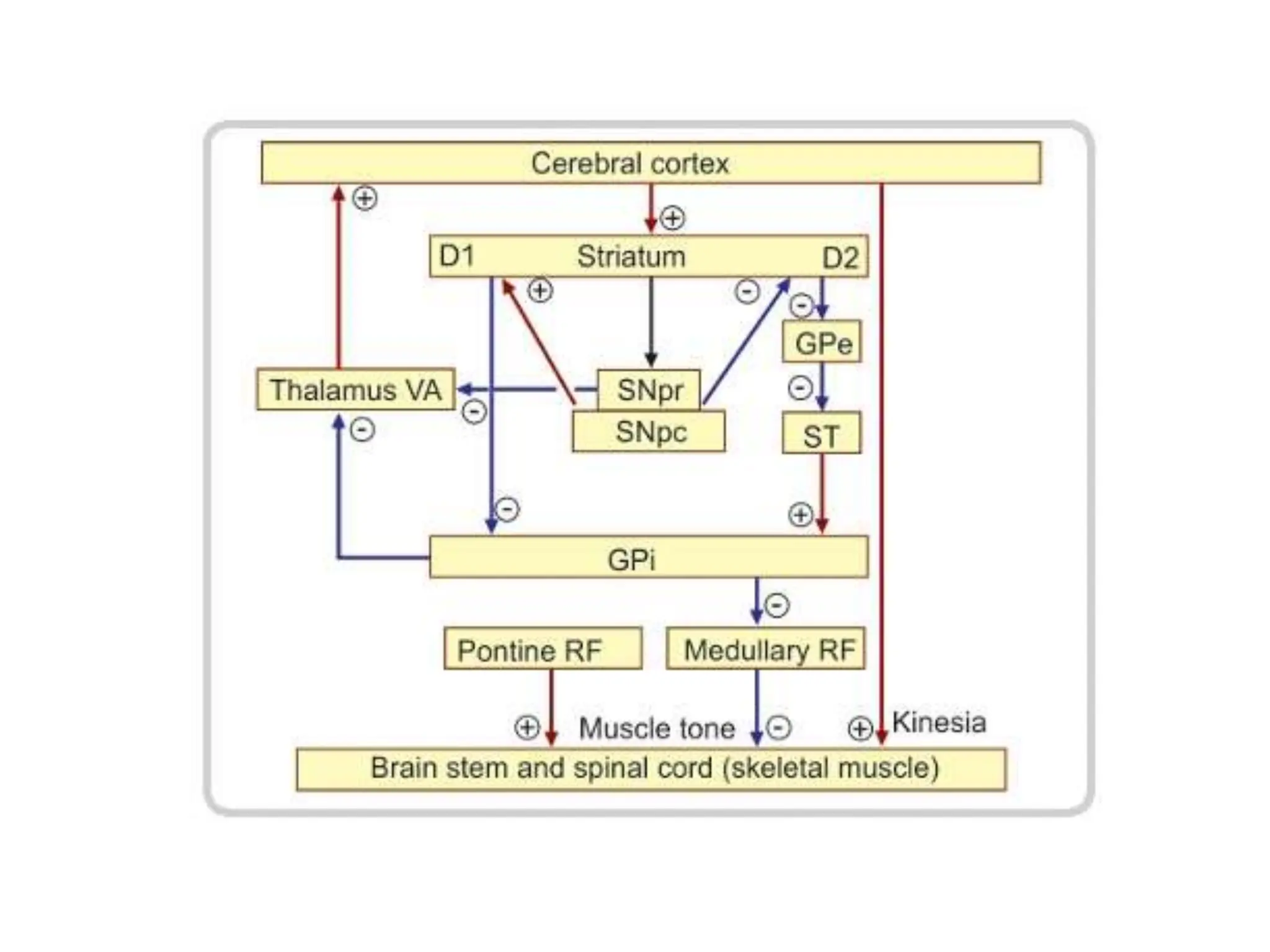
The document provides a detailed overview of the anatomy, functional divisions, and clinical significance of the basal ganglia, including their role in movement and various neuropsychiatric disorders. It describes the various anatomical structures, their relationships, blood supply, and specific pathways involved in motor control, as well as abnormalities associated with conditions like Parkinson's disease, Huntington's disease, and ADHD. Additionally, the document covers how basal ganglia dysfunctions manifest in different movement disorders and their implications in behaviors related to addiction and psychiatric conditions.