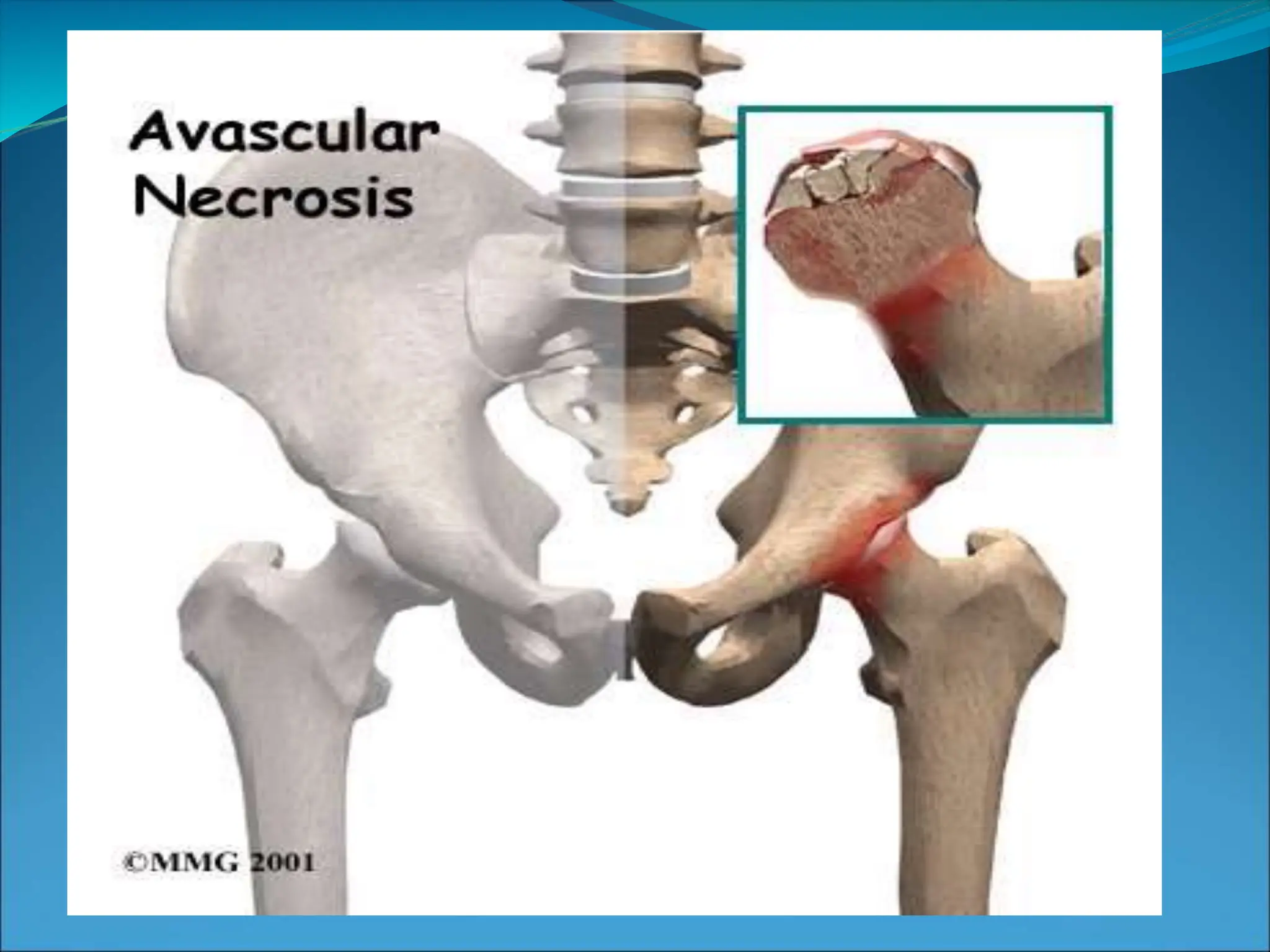
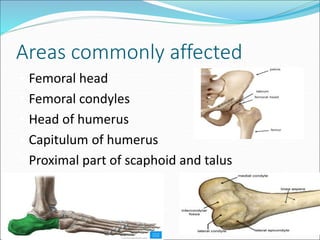
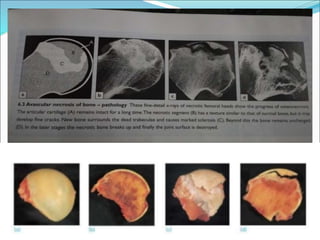
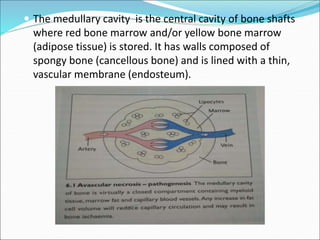
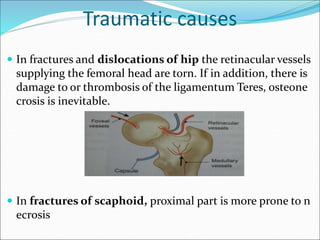
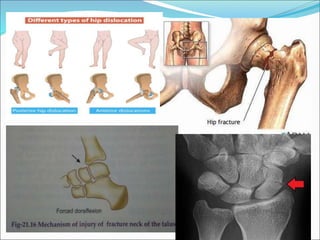
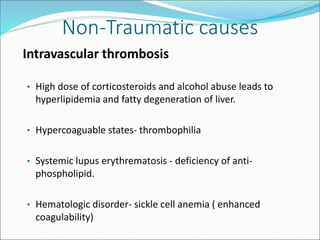
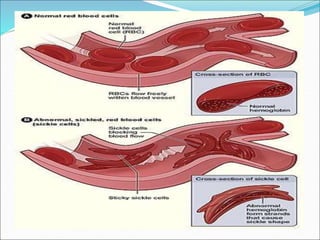
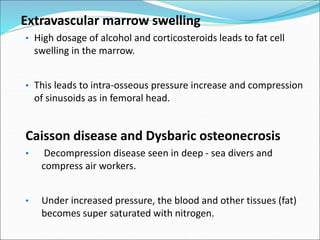
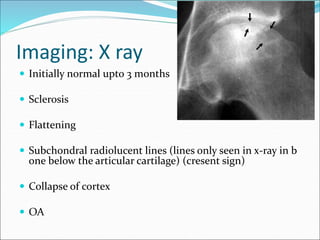
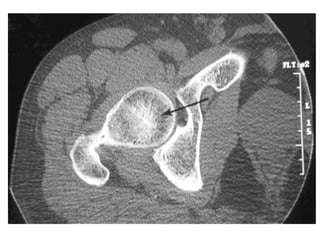
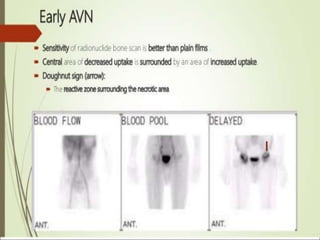
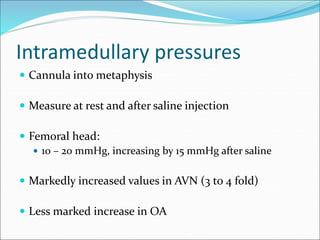
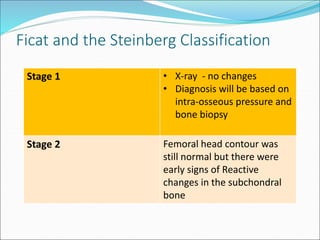
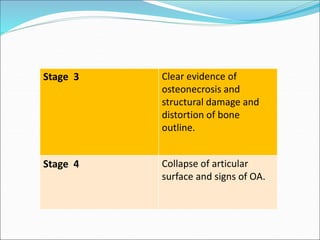
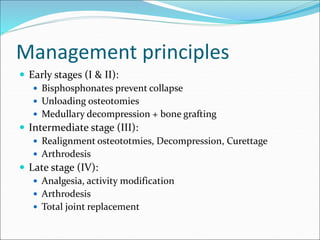
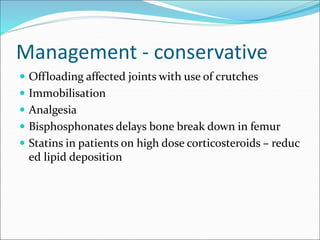
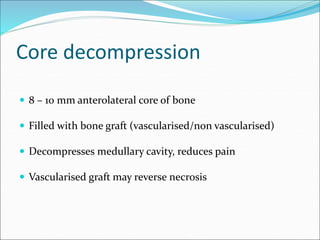
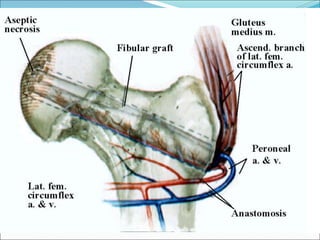
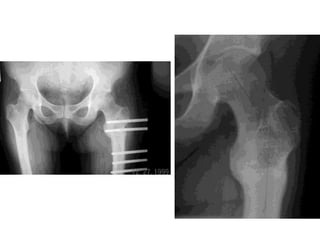
This document discusses avascular necrosis (AVN), also known as osteonecrosis. It begins by defining AVN as the death of bone components due to interrupted blood supply. Key areas that are commonly affected are described. The document then covers the pathophysiology, various causes (traumatic, non-traumatic), clinical presentation, imaging techniques, staging classifications, and management strategies for AVN. Treatment approaches include conservative options, decompression procedures, realignment osteotomies, arthrodesis, and arthroplasty.