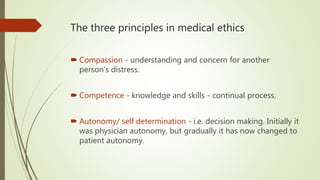
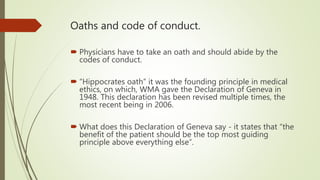
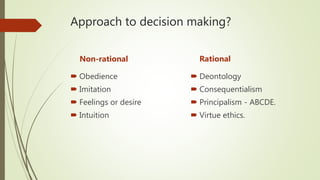
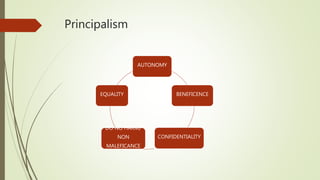
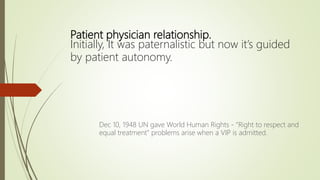
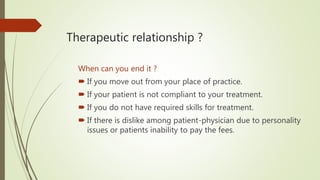
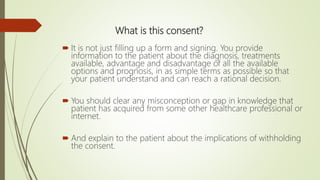
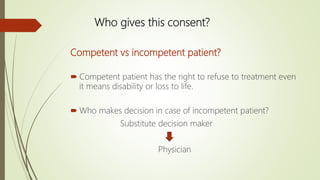
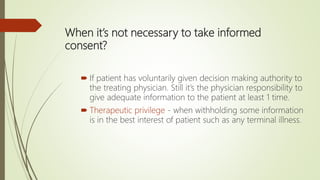
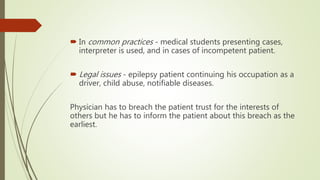
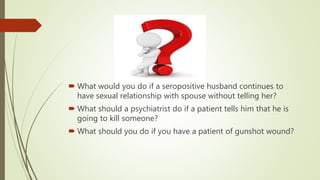
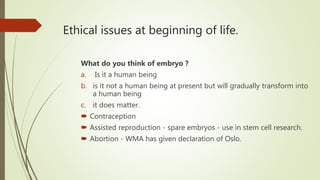
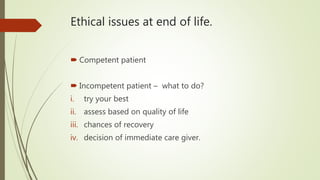
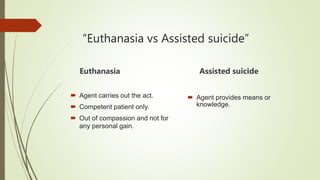
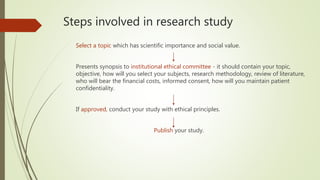
The document is a comprehensive lecture on medical ethics, covering its principles, including compassion, competence, and autonomy, as well as the importance of informed consent and confidentiality. It discusses the roles of the World Medical Association in establishing ethical guidelines, the significance of patient-physician relationships, and various ethical dilemmas faced in medical practice. The lecture emphasizes the need for physicians to navigate complex moral issues while maintaining ethical standards in patient care and medical research.