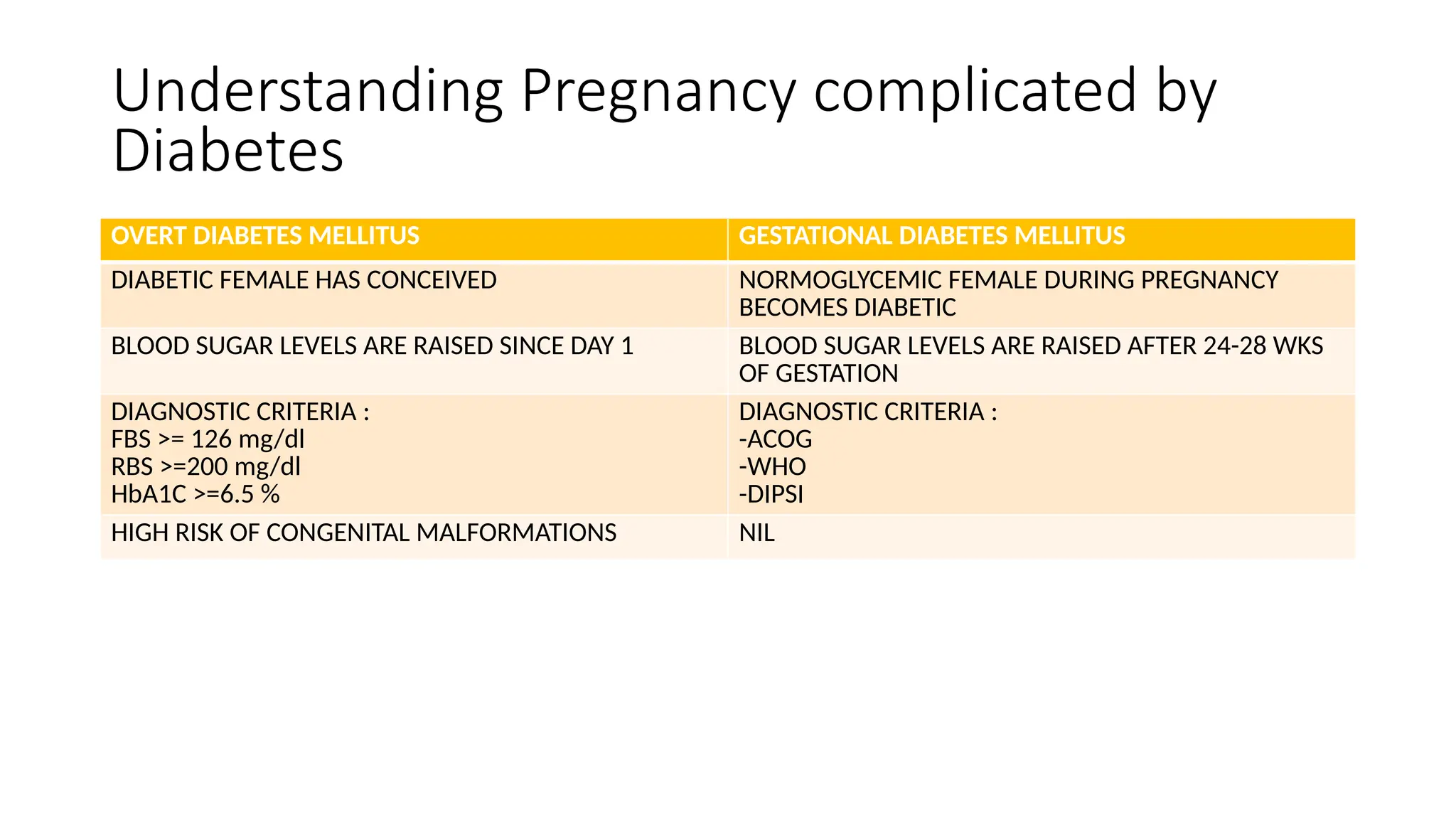
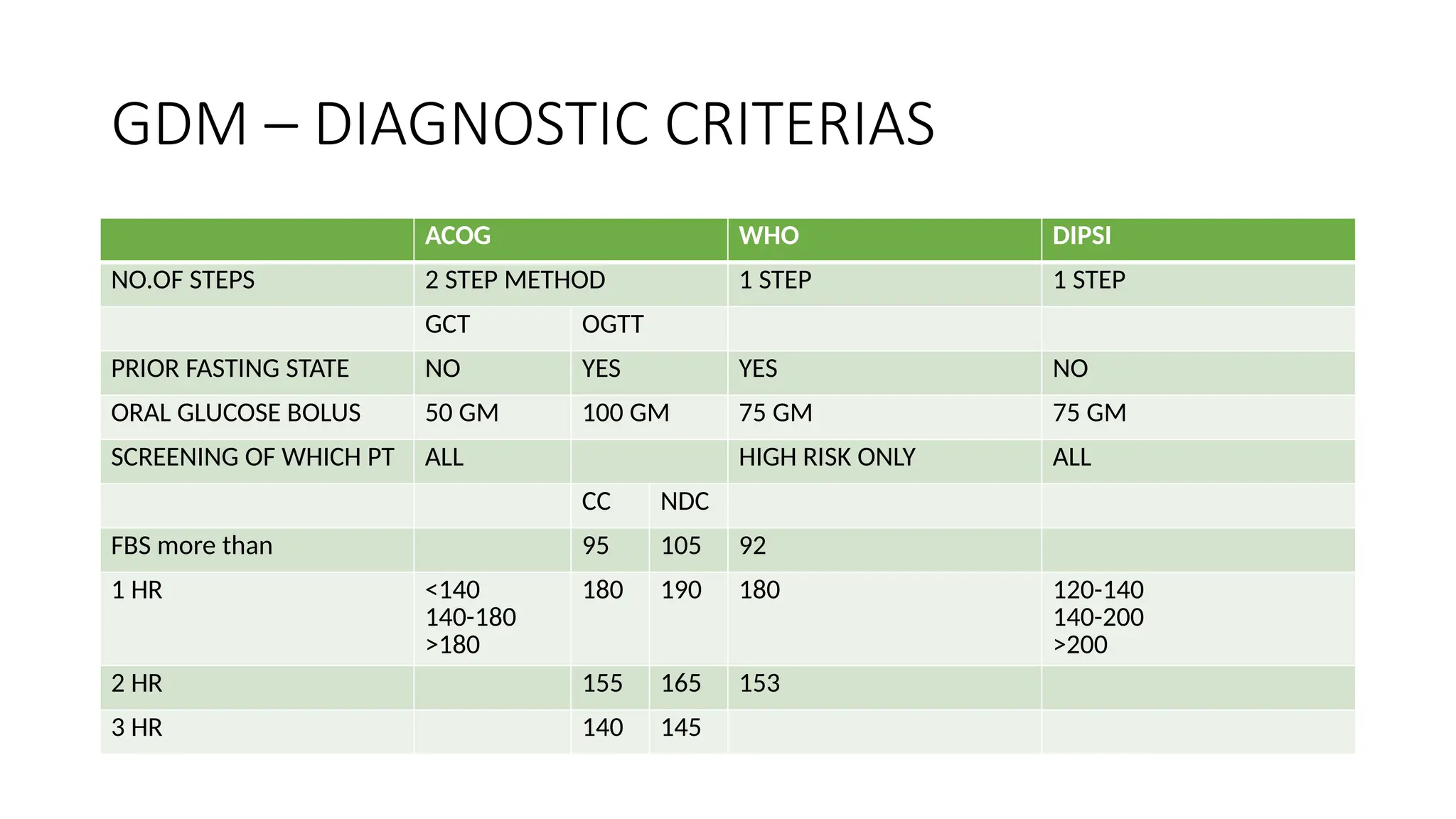
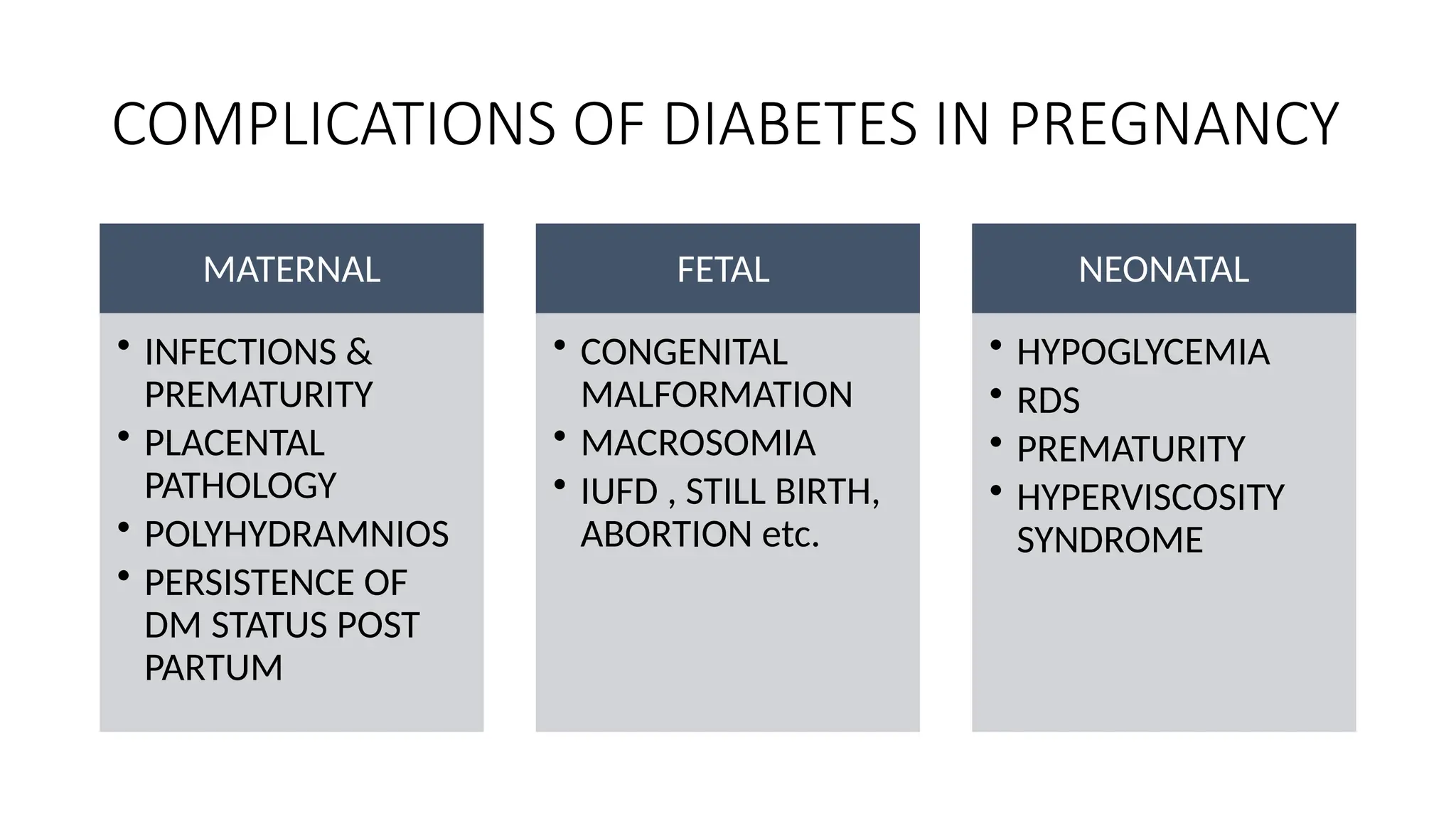
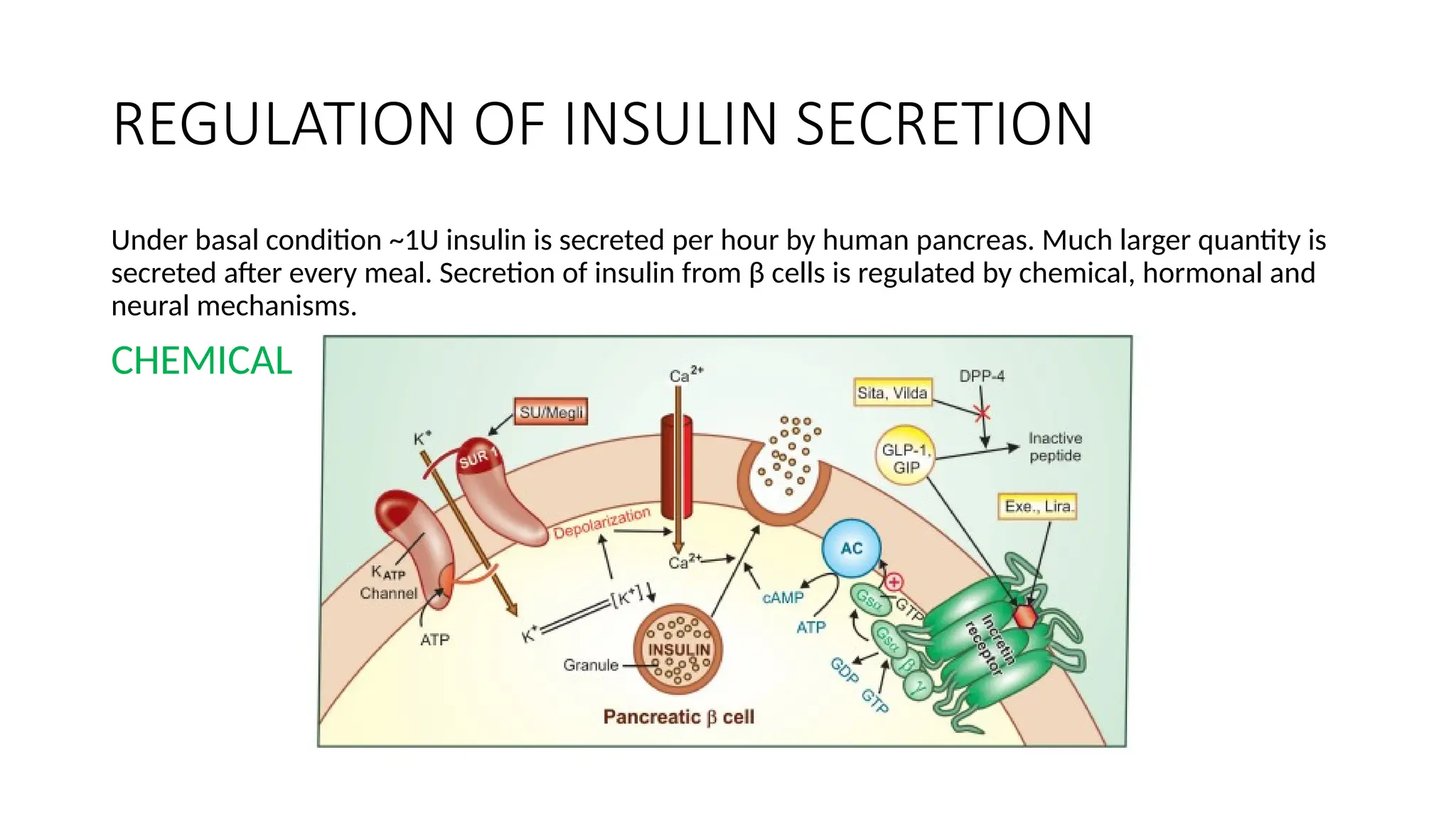
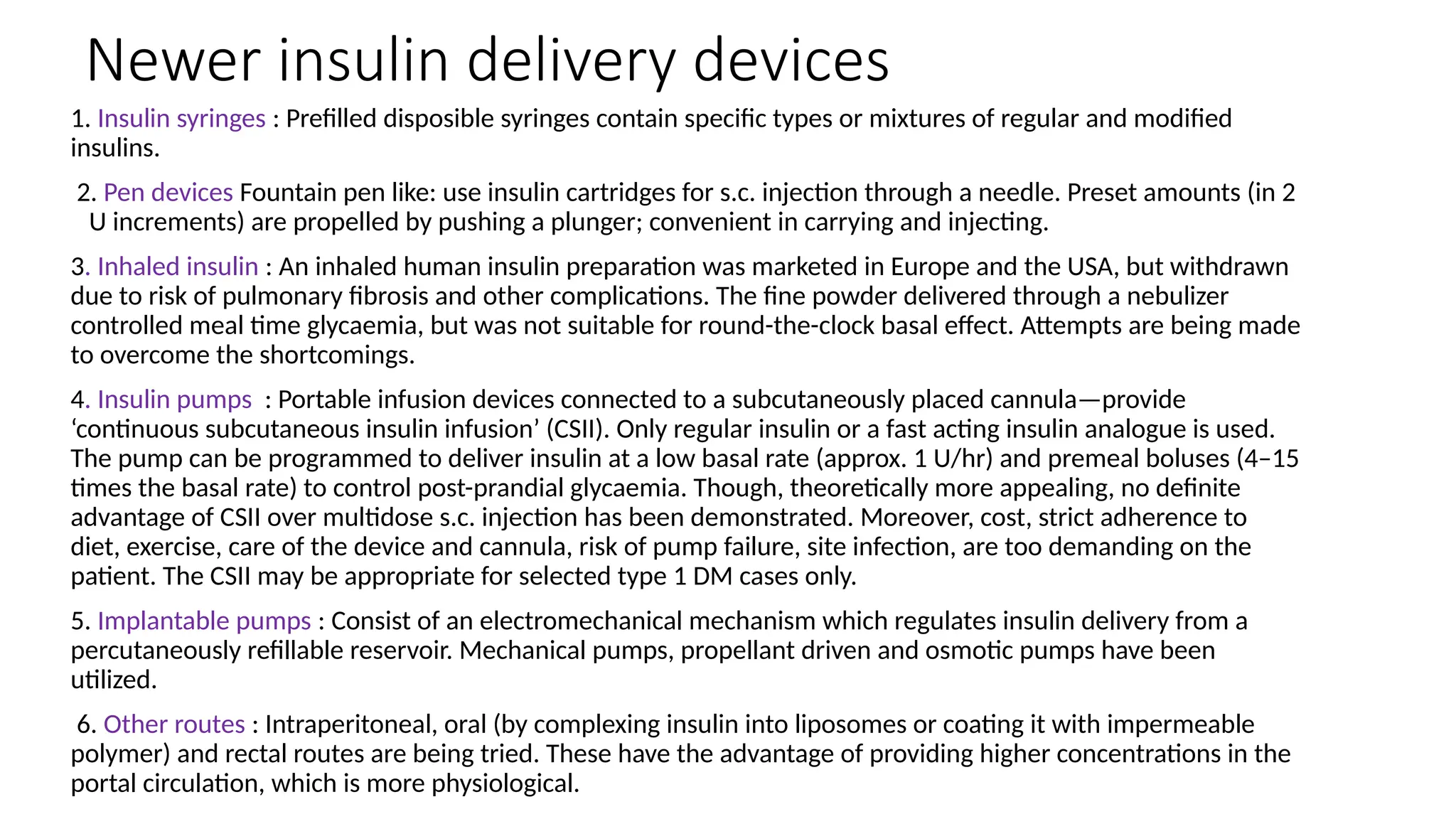
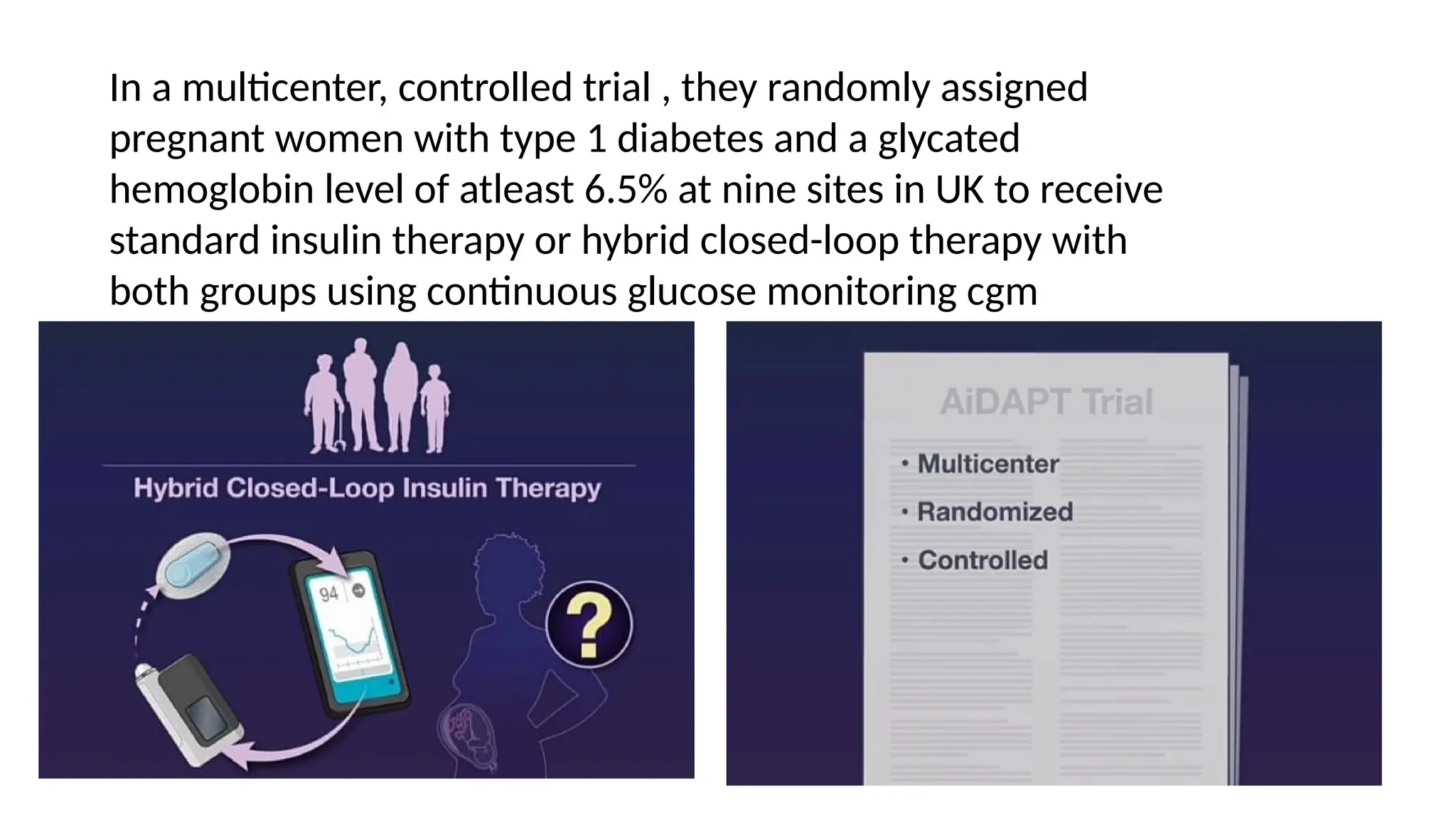
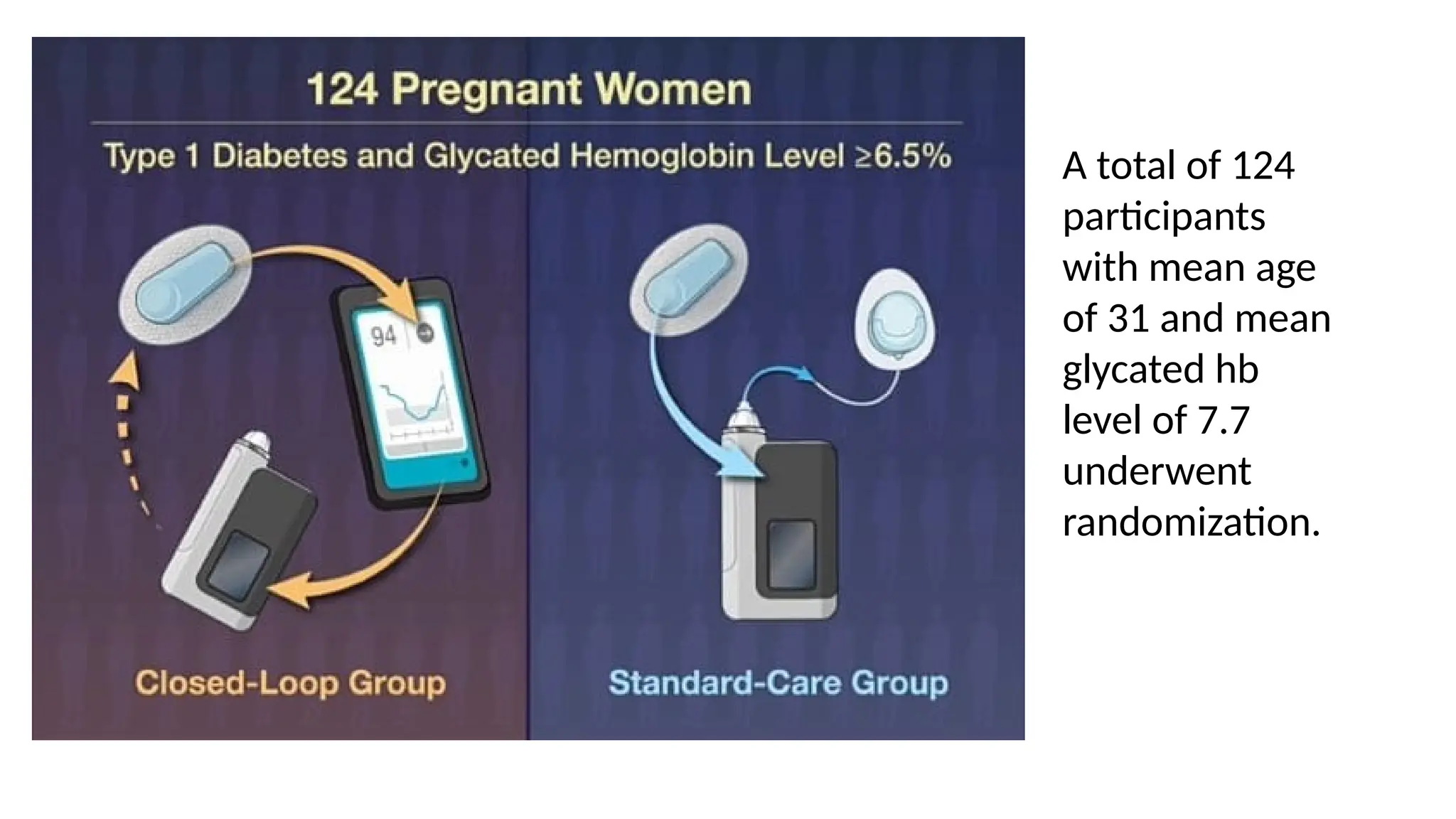
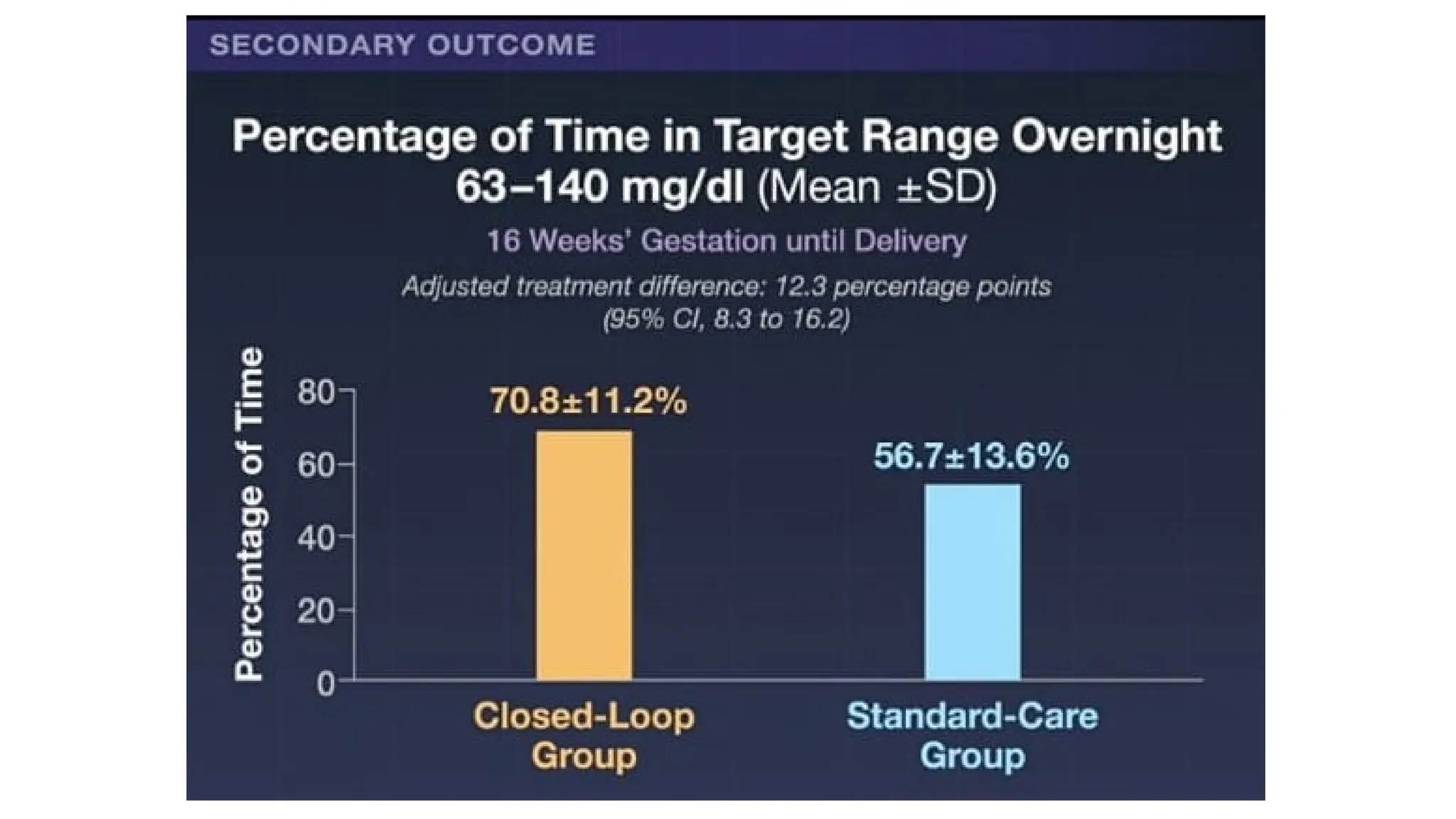
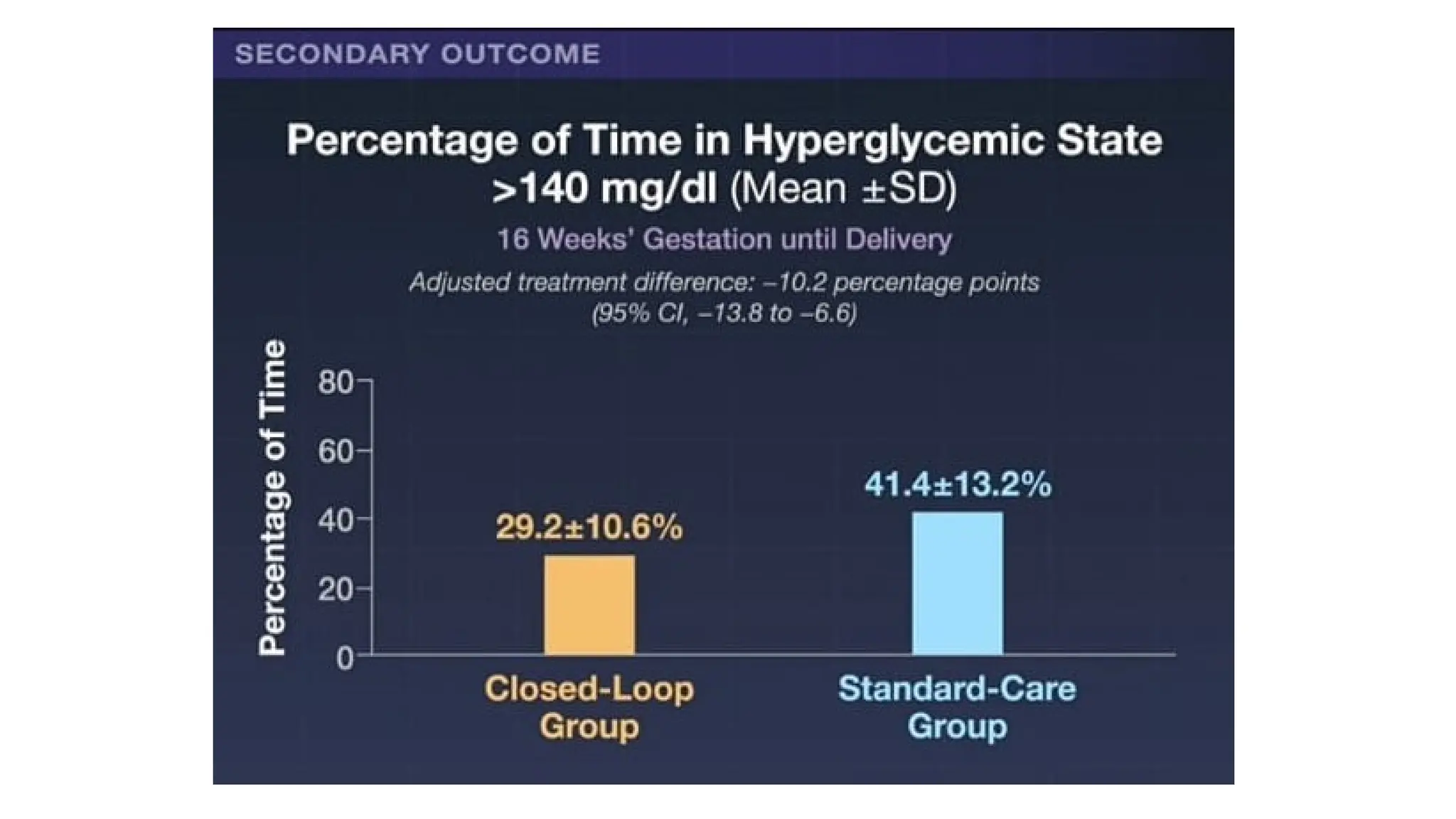
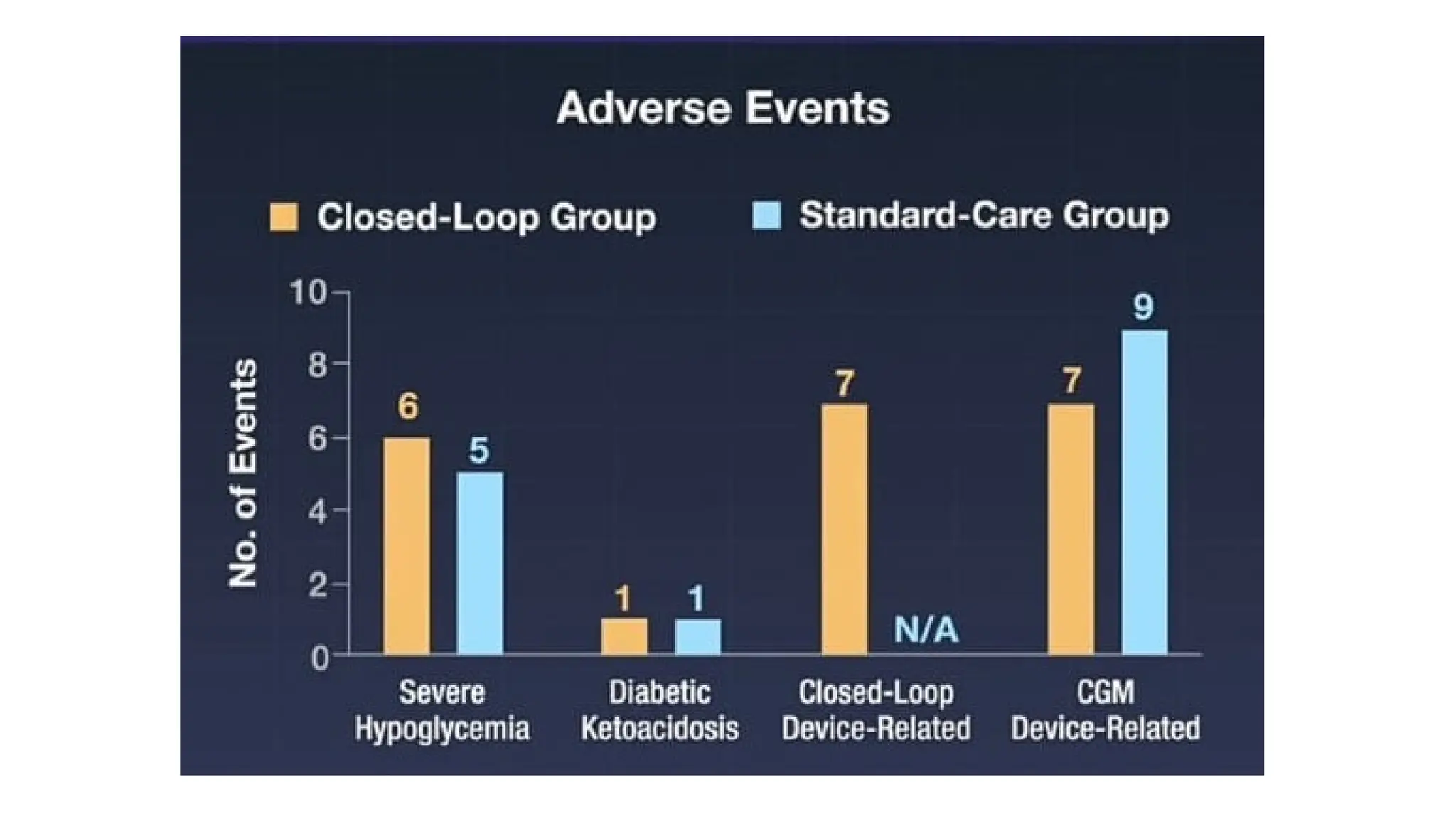
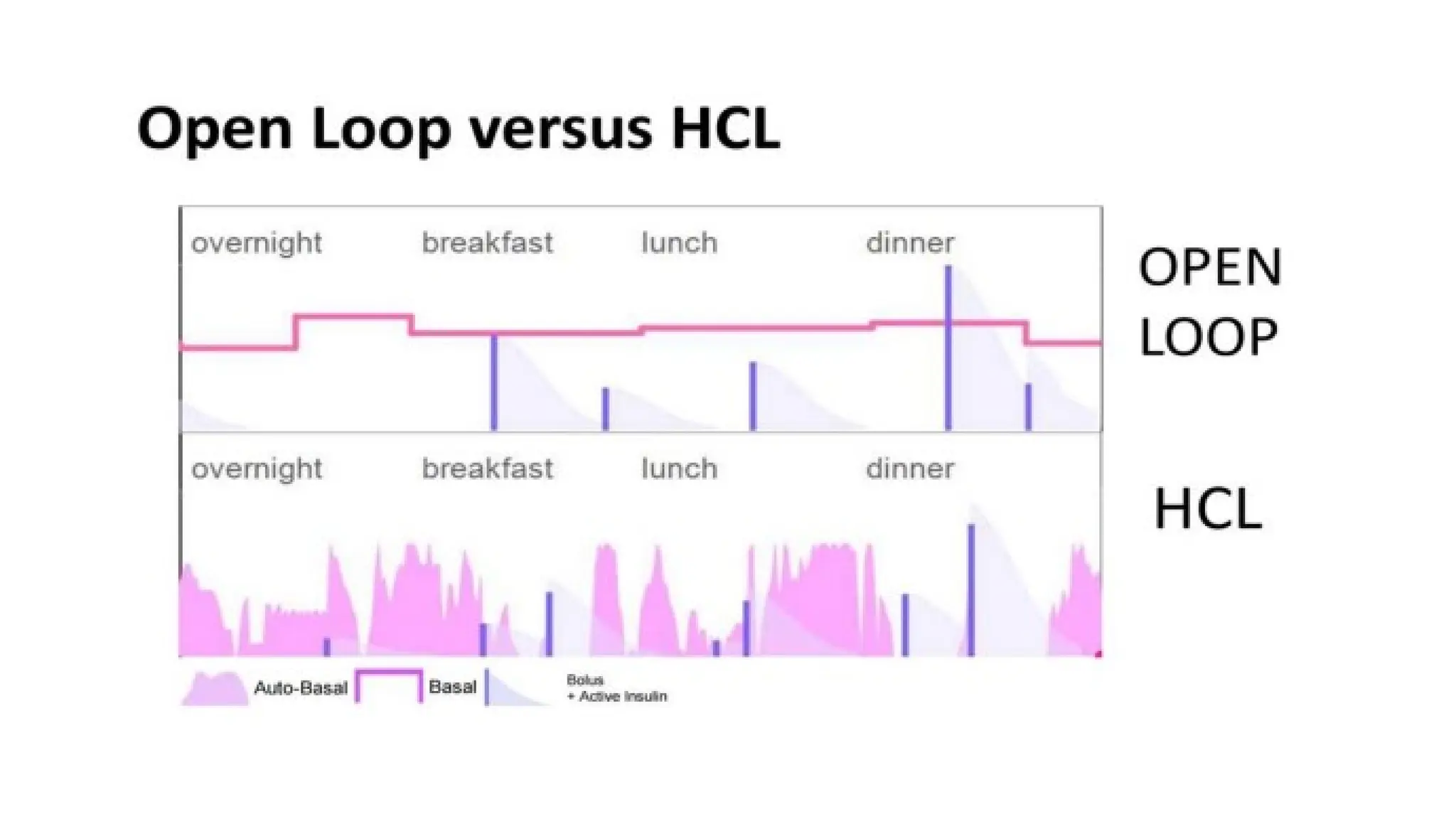
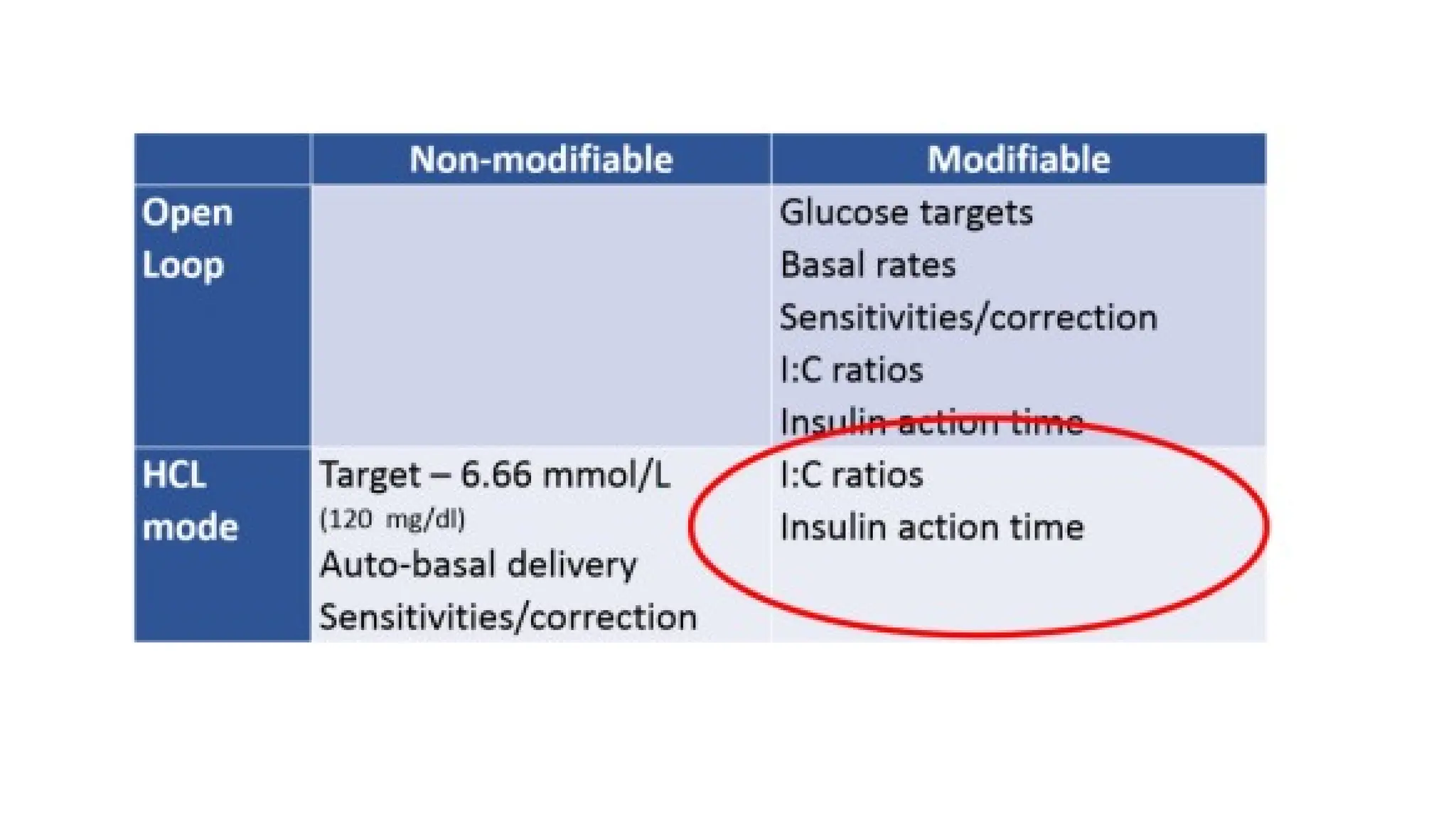
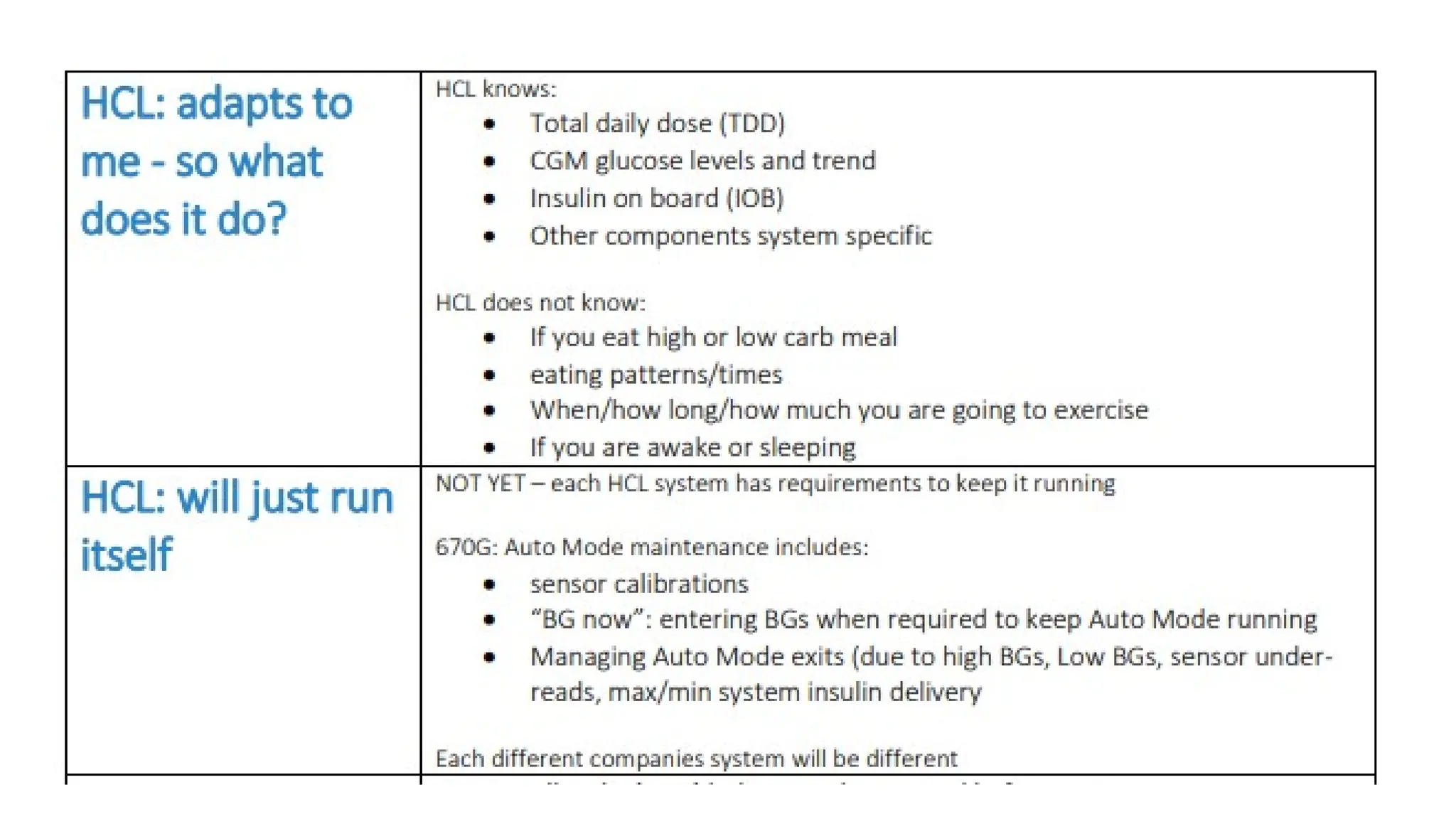
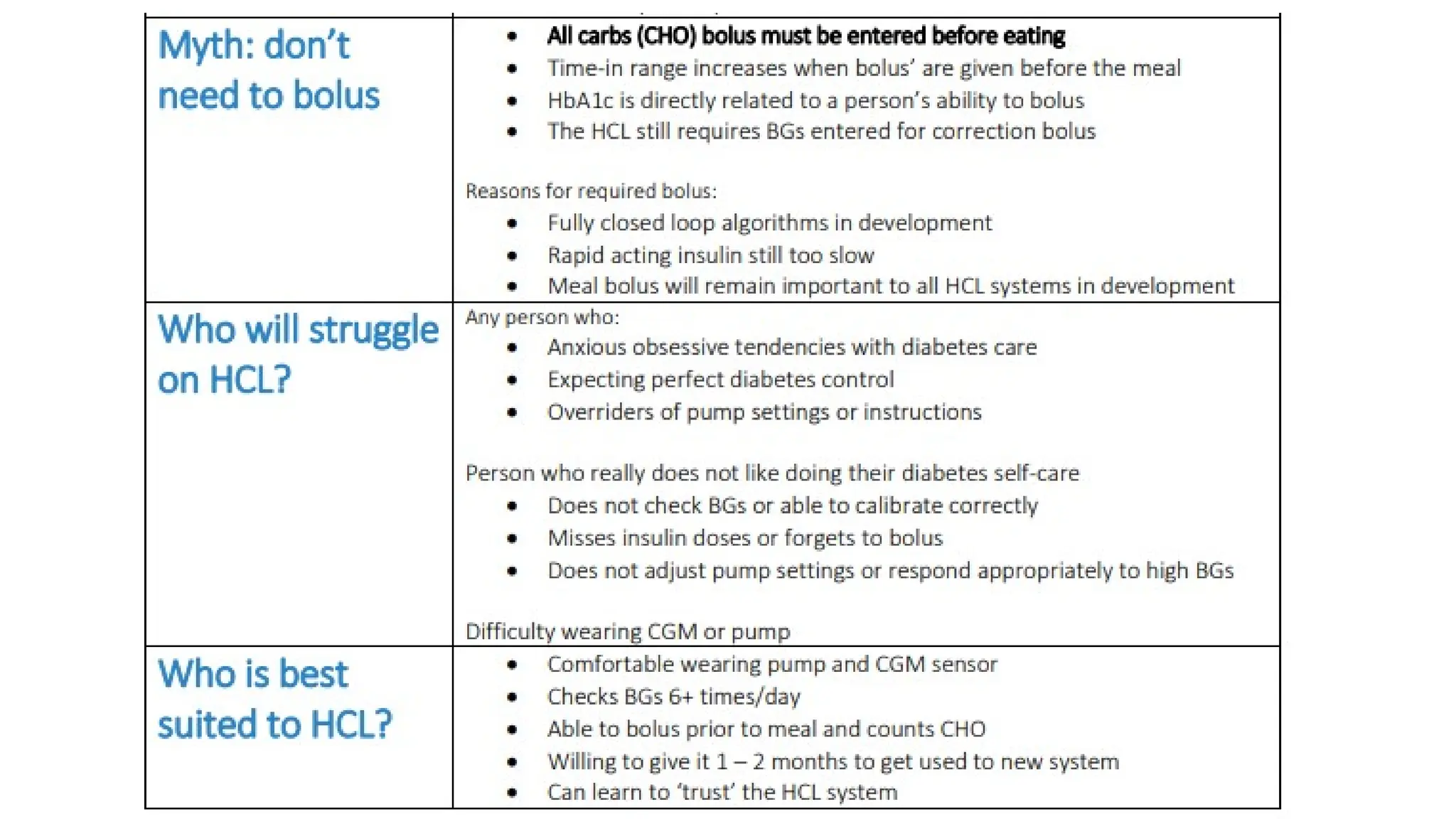
The document discusses automated insulin delivery systems for women with type 1 diabetes during pregnancy, detailing the management of diabetes, insulin delivery methods, and a comparison between traditional and hybrid closed-loop systems. Research indicates that hybrid closed-loop therapy improves maternal glycemic control, while also outlining the benefits and challenges of using such systems. The document concludes that although the current technology is costly and not widely available in India, future advancements may lead to more cost-effective solutions.