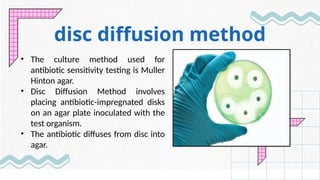
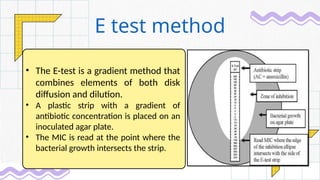
Antibiotic susceptibility testing (AST) determines bacterial sensitivity to antibiotics, guiding effective treatment and managing resistance. Various methods include manual techniques like disc diffusion and broth dilution, as well as automated systems, each with distinct advantages and limitations. AST results inform clinical decisions, enhance patient outcomes, and future advancements like rapid and genotypic testing are anticipated to improve effectiveness against antibiotic-resistant bacteria.