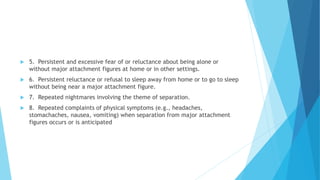
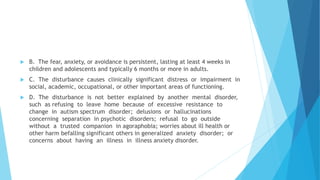
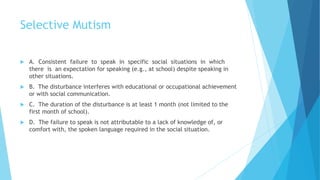
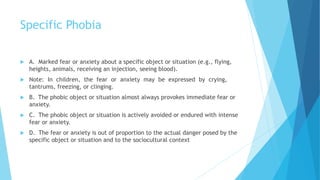
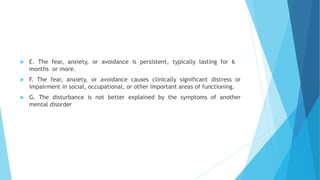
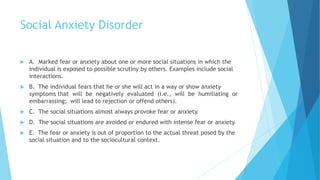
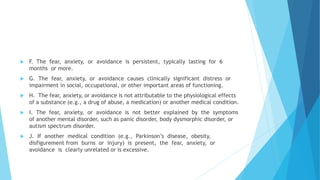
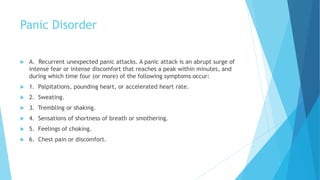
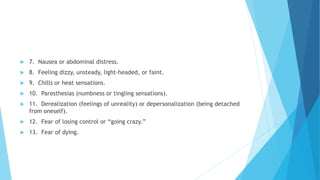
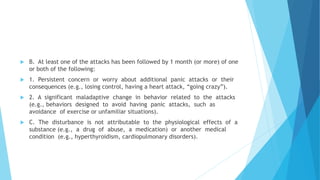
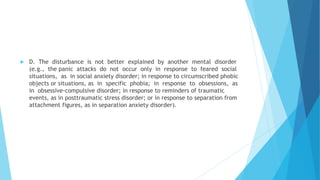
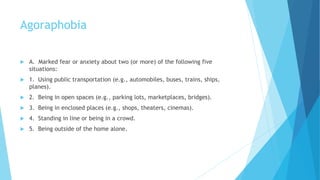
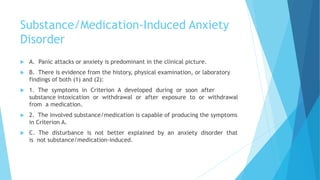
This document provides information on various anxiety disorders. It defines anxiety and discusses when it becomes pathological. It then outlines the physical, cognitive, behavioral, and affective impairments associated with anxiety disorders. The document discusses causes and risk factors, common types of anxiety disorders (including diagnostic criteria), treatments involving pharmacological and non-pharmacological approaches, and substance-induced anxiety disorders.