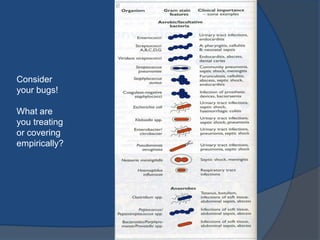
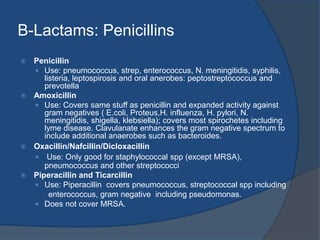
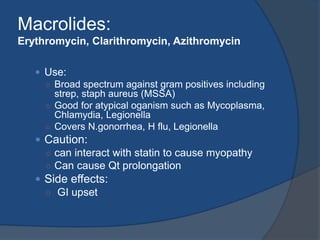
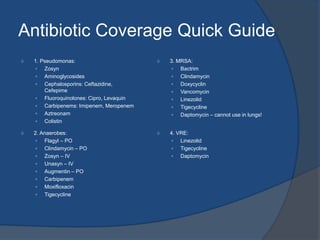
This document provides an overview and guidelines for choosing antibiotics. It discusses collecting cultures before starting antibiotics and ensuring appropriate dosing. Common antibiotics are reviewed including beta-lactams like penicillins, cephalosporins, and carbapenems as well as quinolones, macrolides, and metronidazole. Specific coverage and cautions are highlighted. A case of possible osteomyelitis in a diabetic man with leg cellulitis is presented. Factors to consider when selecting antibiotics include patient history, location of infection, and likely pathogens.