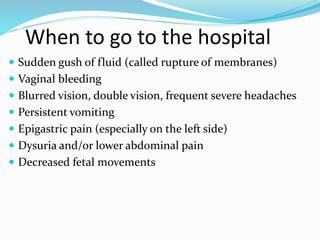
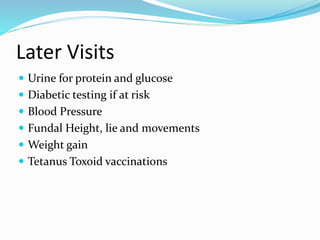
Antenatal care involves regular checkups during pregnancy to monitor the health of the expectant mother and baby. It includes health education, screening for issues like anemia, and preparing the mother for childbirth. Prenatal visits should occur monthly during the first two trimesters, every two weeks during the third trimester, and weekly at the end of the pregnancy. Antenatal care aims to promote health and ensure safe deliveries.