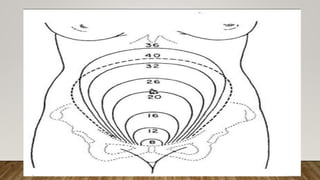
A normal pregnancy lasts about 40 weeks or 280 days. During this time, the fertilized egg implants in the uterus and develops into a fetus. The woman's body undergoes many physiological changes to support the growing fetus. These include enlargement and thickening of the uterus; increased blood volume, cardiac output and iron levels; and softening of tissues in preparation for childbirth. The fetus is nourished through the placenta and surrounded by amniotic fluid and membranes within the uterus.