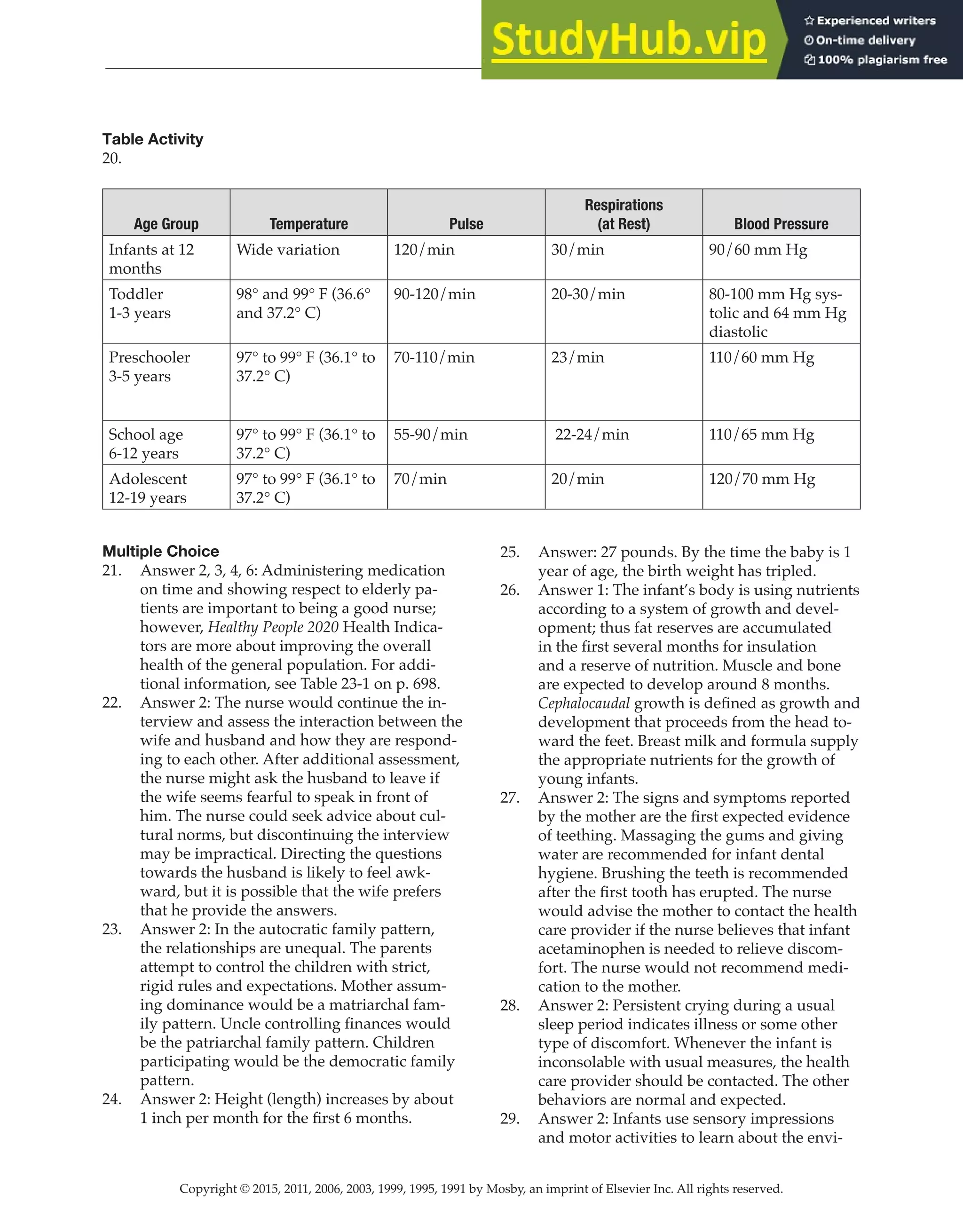
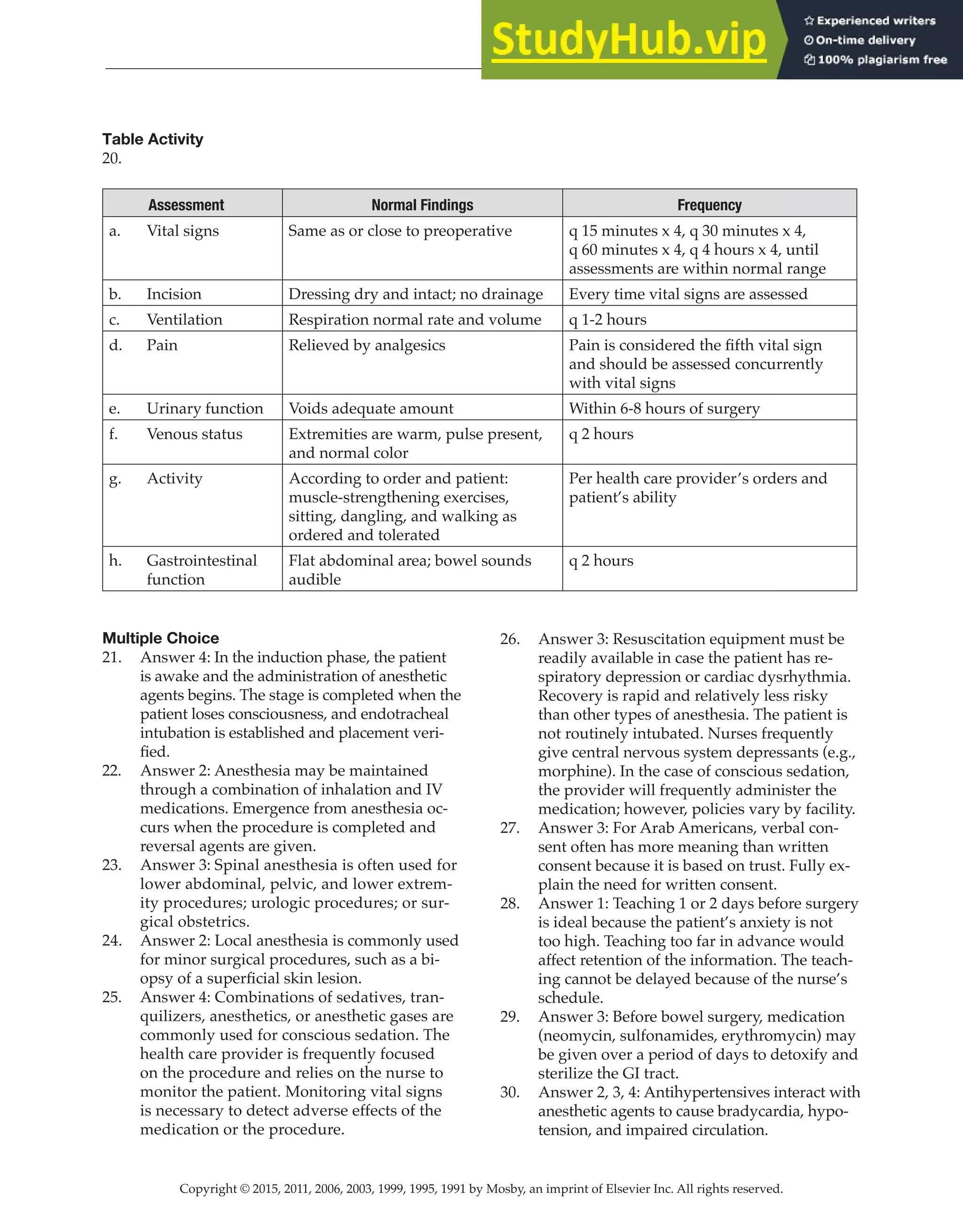
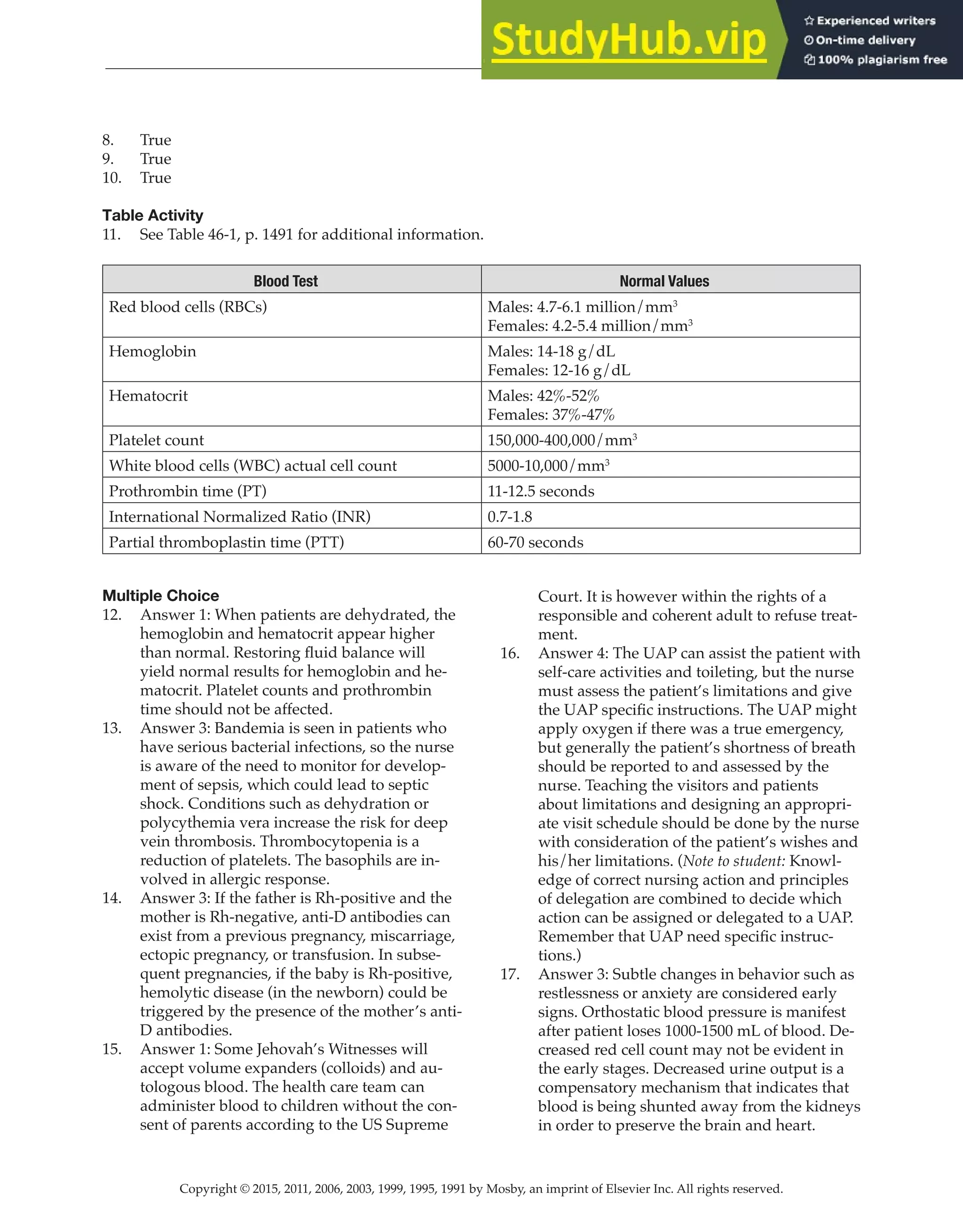
This document provides an answer key for a nursing textbook chapter on the evolution of nursing and legal/ethical aspects of nursing. It includes answers to matching, short answer, fill-in-the-blank, multiple choice and critical thinking questions related to the content in the two chapters. The answer key is copyrighted material from Elsevier intended to accompany the textbook chapters.

![Copyright © 2015, 2011, 2006, 2003, 1999, 1995, 1991 by Mosby, an imprint of Elsevier Inc. All rights reserved.
Answer Key
11
new assessment data, the care plan may
have to be modified.
27. Environment—the nurse is experiencing
an overload of distraction from a variety of
sources. The nurse’s posture and position
(crossing the arms over the chest) and the
space and territory (standing too far away
and by the door) convey impatience. The
message to the patient is “I do not want to
communicate with you.” Any trust between
the nurse and patient is destroyed. “Dear” is
used less by younger people and possibly the
nurse may view “dear” as condescending.
The patient may be experiencing unresolved
grief over the loss of husband (recall that she
is a widow) or stress related to hospitaliza-
tion. The patient could also be having a physi-
ologic problem such as fever or an electrolyte
imbalance which has triggered confusion or
hallucinations. Cultural differences and use of
language could also be factors. For example,
the patient may not be able to directly express
fears and concerns, so repeatedly uses the call
bell to get attention.
28. See Table 4-4, p. 73.
We all use responses that block commu-
nication, so do not judge yourself to be a poor
communicator if you have numerous exam-
ples.
On the other hand, if you cannot think of
any examples where you used responses that
blocked communication, you may need to in-
crease awareness of what you are saying and
how others are responding to you. Conscious
use of communication responses and the ef-
fect that responses have on others allow us to
intentionally improve our therapeutic com-
munication.
CHAPTER 5—NURSING PROCESS AND
CRITICAL THINKING
Crossword Puzzle
1. See Table 5-3, p. 82.
A
4
N
T
I
8
C
I
P
A
T
O
R
Y
N
F
1
U
N
C
T
I
O
N
A
L
12
D
14
E
O
E
D
5
R
W
L
Y
R
A
S
U
S
11
Y
F
P
I
E
U
T
T
D
N
E
U
C
D
9
I
S
A
B
L
I
N
G
T
T
I
I
6
N
A
B
I
L
I
T
Y
I
16
O
O
N
N
D
7
E
10
F
E
N
S
I
13
V
E
15
E
A
F
A
M
X
F
L
F
L
P
C
F
E
A
E
E
C
I
S
C
T
R
S
T
A
2
B
I
L
I
T
Y
E
I
I
V
D
V
V
P
3
E
R
C
E
I
V
E
D
E
E
True or False
2. True
3. False. Identification of problems occurs dur-
ing the diagnosis phase.
4. False. A nursing intervention is created to
provide specific written instructions for all
caregivers.
5. False. Advising patients about medications
for a health condition is the responsibility of
the health care provider.
6. False. Perceived constipation is defined as
“self-diagnosis of constipation and abuse of
laxatives, enemas, and/or suppositories to en-
sure a daily bowel movement.”
Short Answer
[Note to the student: For questions 7, 8, 9, and 10,
the answer key shows examples of nursing diagno-
ses, goals, interventions, or evaluation statements.
Your answers may differ, so check your answers for
these questions against the following criteria. The
nursing diagnosis should include: (1) the nursing
diagnosis label from the NANDA-I list; (2) the
contributing, etiologic, or related factor; and (3)
the specific cues, signs, and symptoms from the
patient’s assessment. A patient outcome statement
provides a description of the specific, measurable
behavior (outcome criteria) that the patient will be
able to exhibit in a given time frame following the
interventions. Nursing actions should be directly
related to helping the patient achieve the goal
and evaluation statements should reflect achieve-
ment, partial achievement, or failure to achieve the
patient-centered outcome.]](https://image.slidesharecdn.com/answerkeystudyguide-230807165434-b863724b/75/Answerkeystudyguide-pdf-11-2048.jpg)