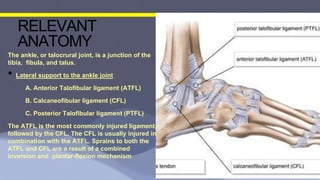
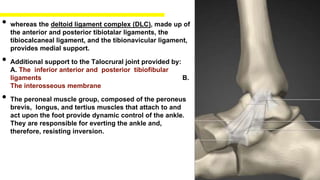
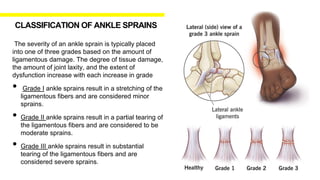
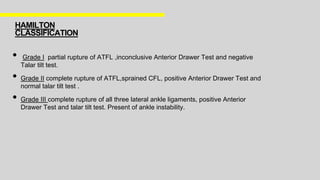
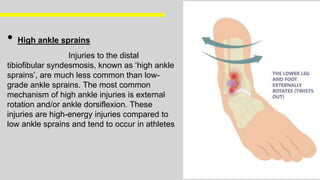
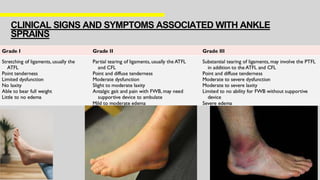
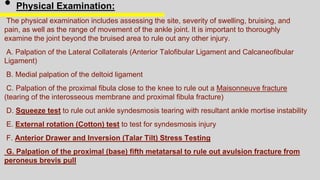
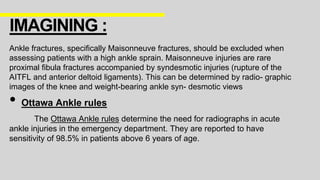
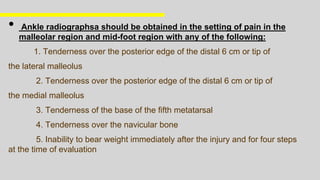
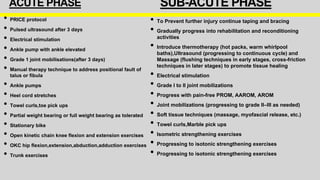
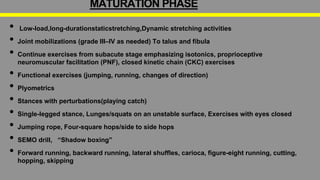
Ankle sprains are prevalent injuries, particularly among athletes aged 10 to 19, with various grades of severity based on ligament damage. Proper management, including rehabilitation and reconditioning, is critical to prevent reinjury and chronic dysfunction. Assessment and imaging protocols, such as the Ottawa ankle rules, play vital roles in treatment planning.