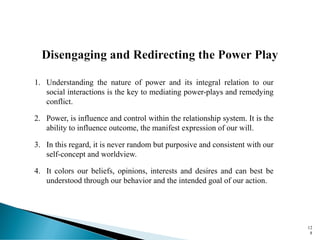
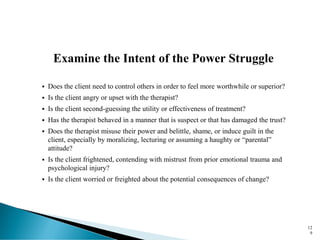
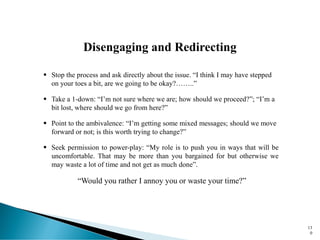
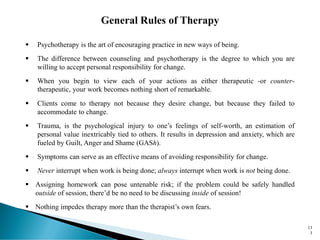
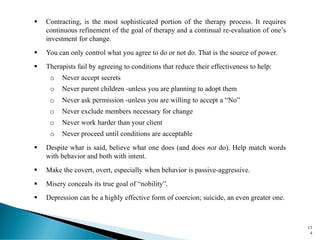
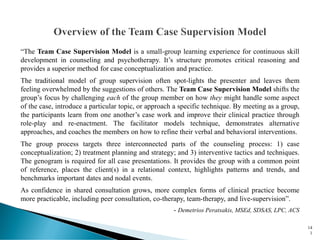
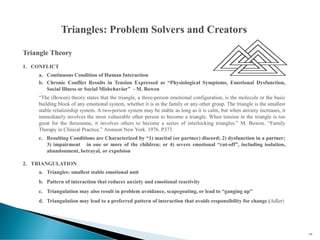
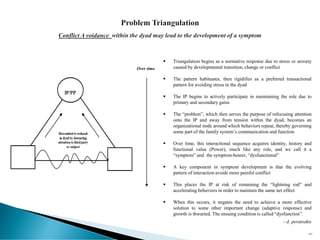
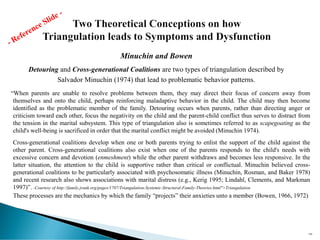
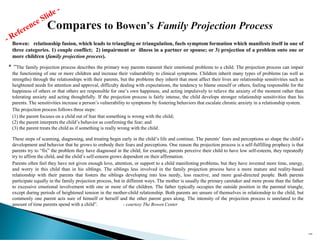
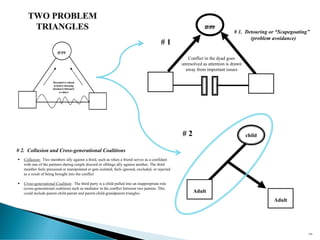
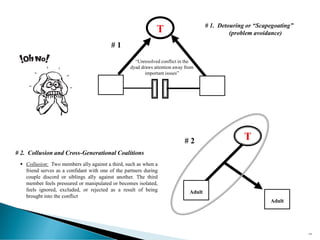
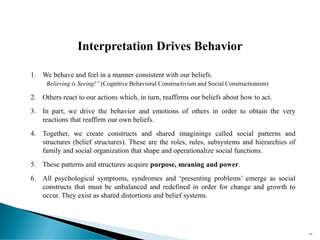
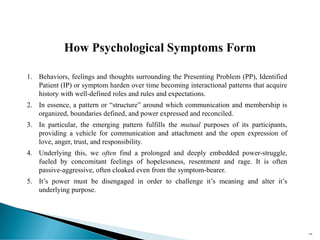
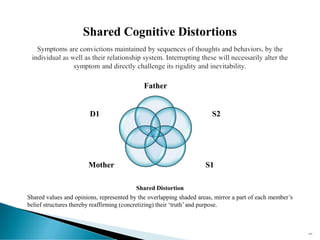
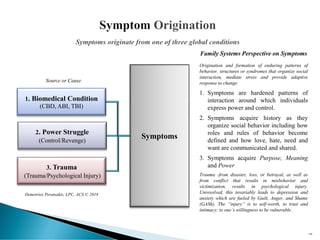
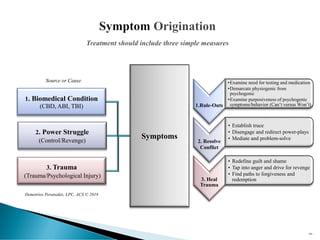
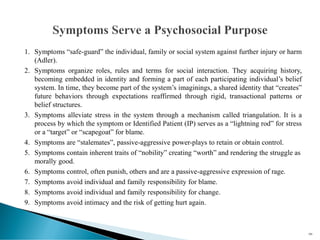
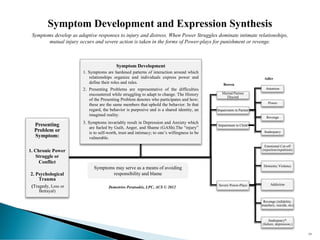
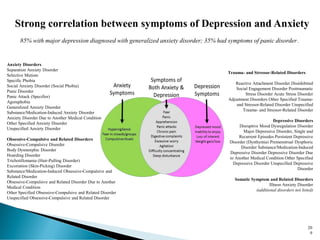
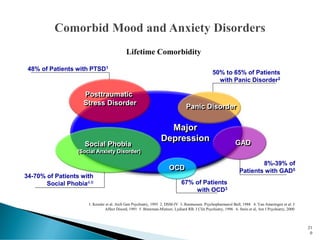
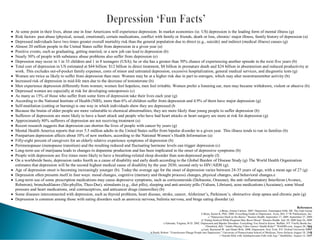
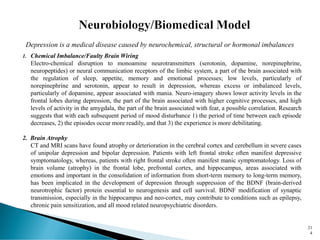
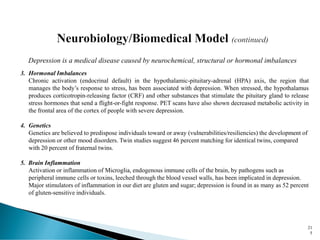
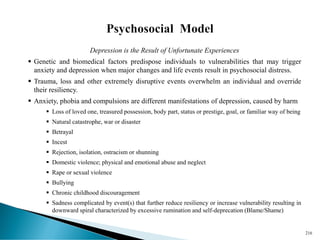
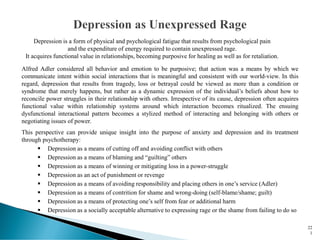
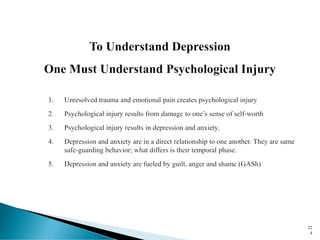
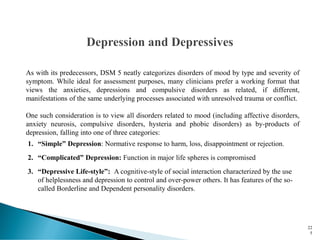
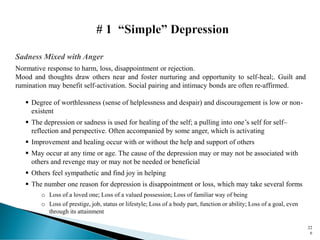
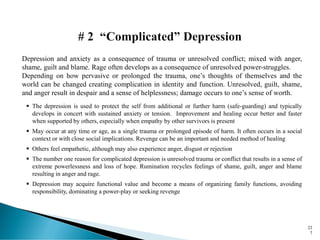
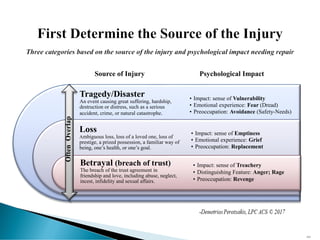
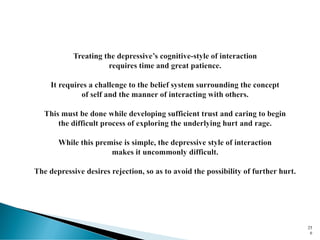
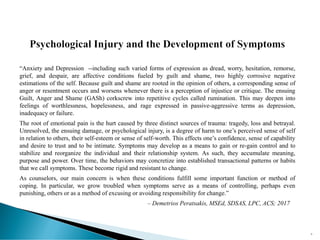
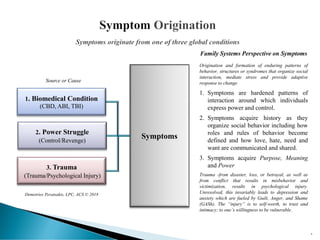
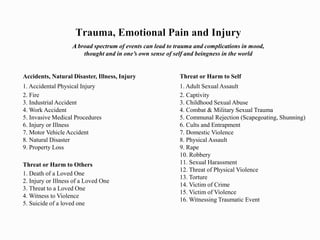
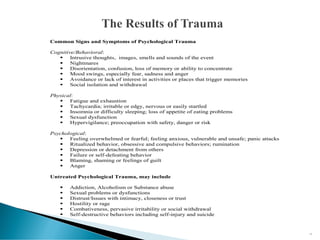
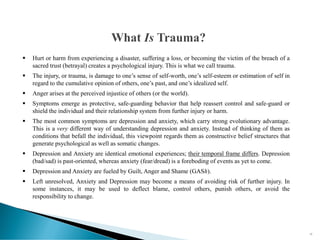
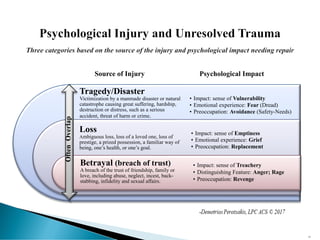
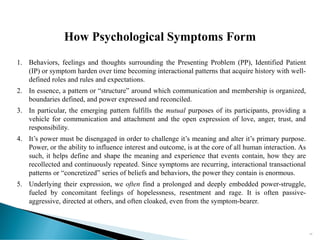
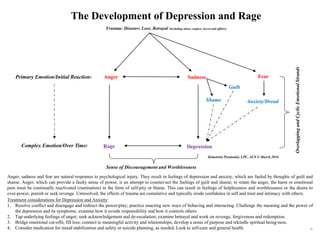
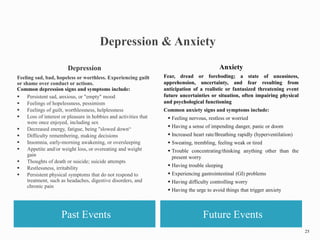
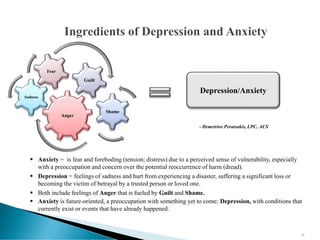
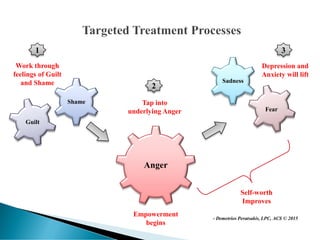
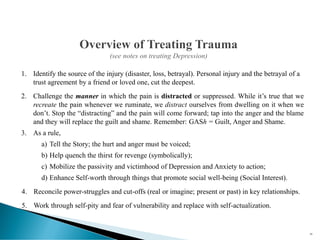
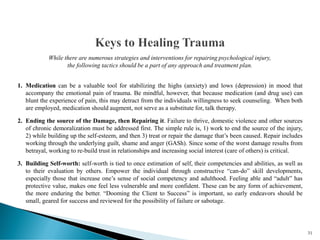
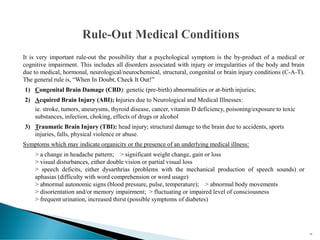
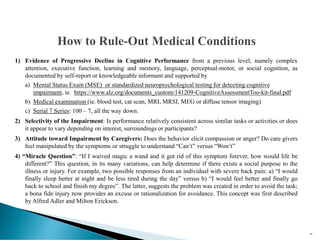
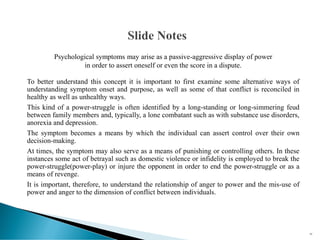
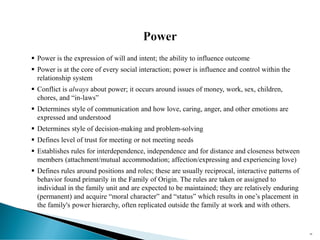
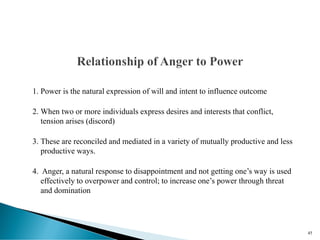
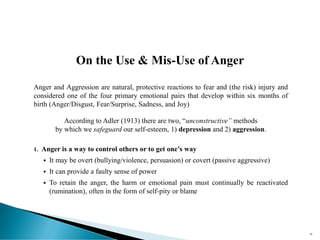
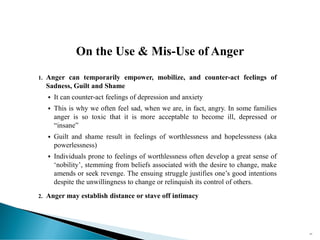
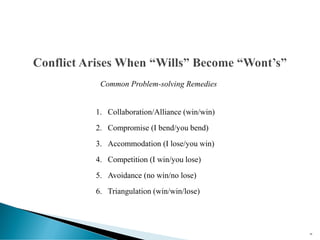
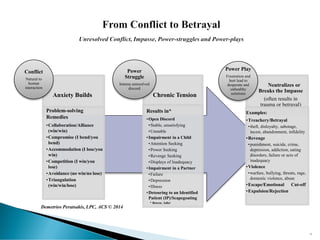
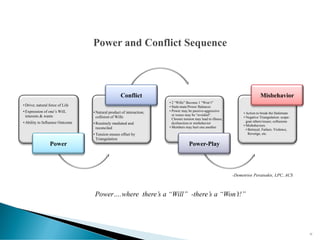
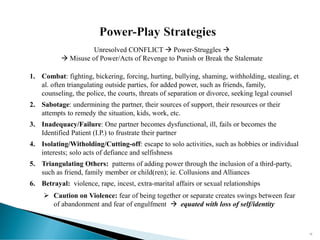
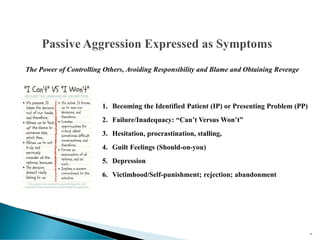
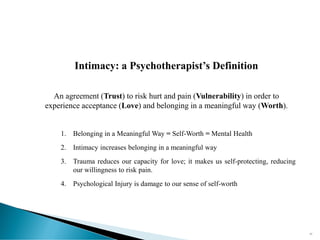
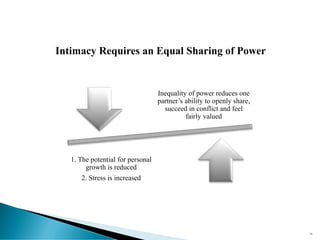
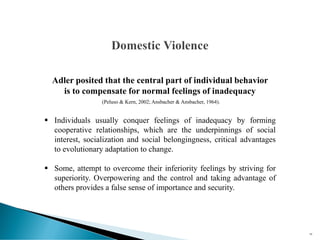
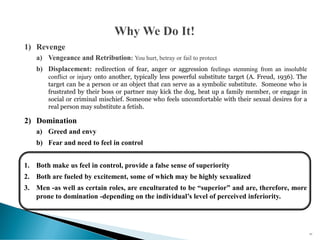
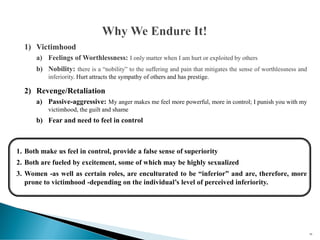
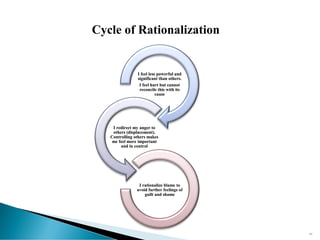
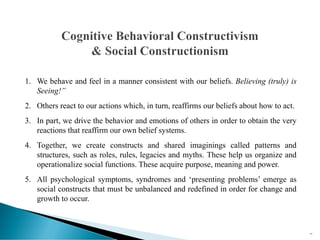
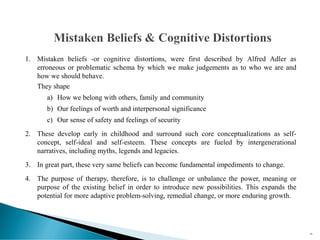
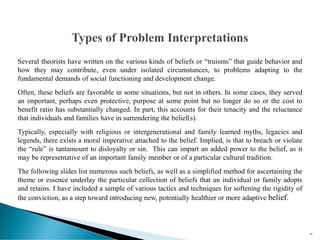
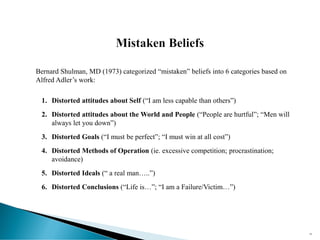
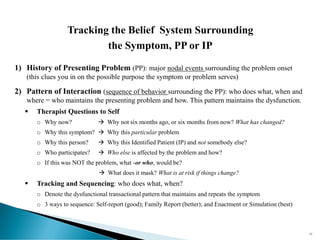
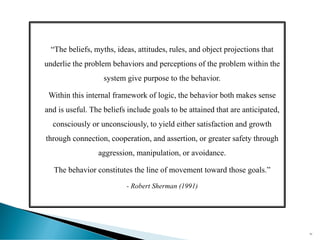
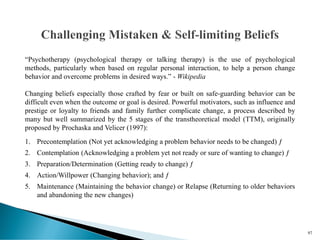
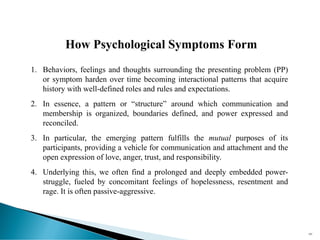
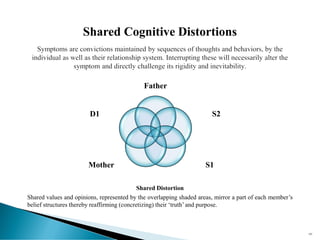
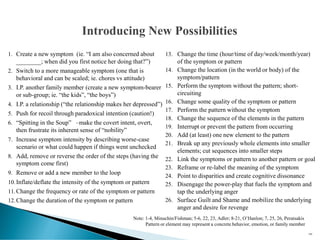
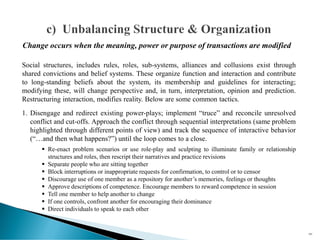
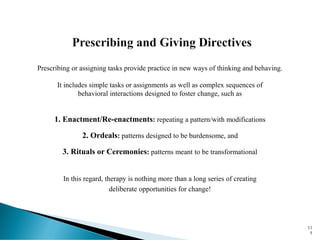
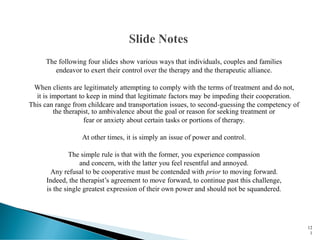
The document discusses the philosophy and practice of clinical outpatient therapy from the perspective of Demetrios Peratsakis. It provides an overview of Peratsakis' training and mentors in family therapy and Adlerian approaches. The document also outlines a psychosocial, constructivist perspective on the development of psychological symptoms, viewing them as protective belief structures that arise from trauma, power struggles, or medical conditions. It discusses how symptoms acquire meaning, purpose, and power over time through hardened interaction patterns. Unresolved trauma can result in depression and anxiety, which are fueled by guilt, anger, and shame and left untreated, may be used to control or punish others.










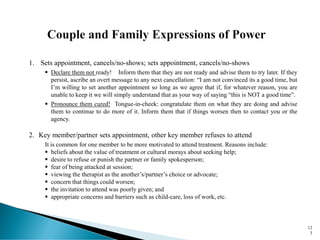
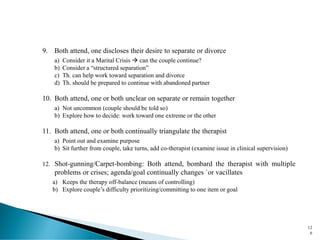
![1. Not talking
2. Not following advice or
suggestions
3. Non-disclosure [Selective
disclosure] or not answering
questions
4. Taking notes or recording sessions
5. Coming late or leaving sessions
early
6. Non-payment/Non-compliance
with Required releases and
Paperwork
7. Stalking, Threatening, or
Intimidating
8. Provocative or threatening clothing
9. Change seating or other office
arrangements
10. Provocative or threatening language
11. Use of language
12. Belligerence and Rage
13. Dominating the conversation
14. Inappropriate touching, hugging, etc
15. Inappropriate gifts
16. Inappropriate or offering incentives
17. Acting seductively, coy or unduly
vulnerable
12
2
1-17: “Client Expressions of Power in the Therapeutic Alliance” -by Ofer Zur, P.D.](https://image.slidesharecdn.com/advancedmethodsinclinicalpracticefeb2020-200222015339/85/Advanced-Methods-in-Clinical-Practice-feb-2020-122-320.jpg)