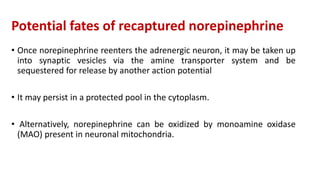
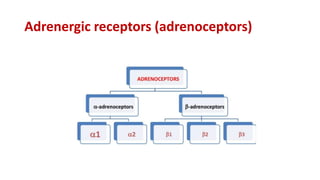
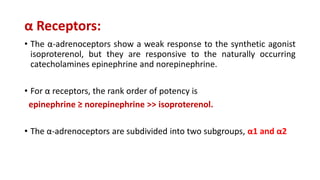
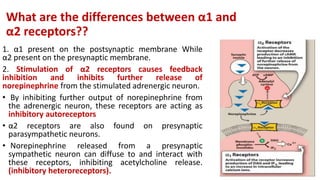
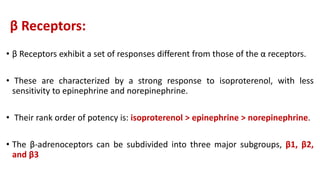
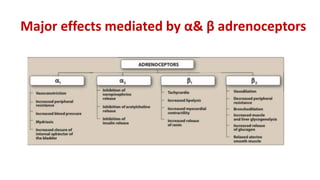
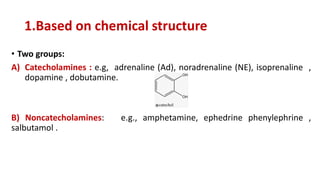
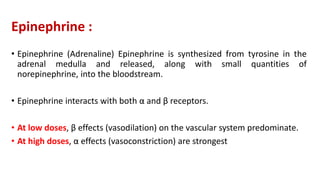
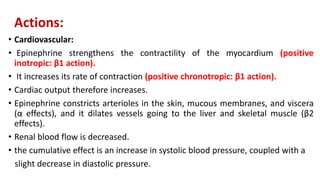
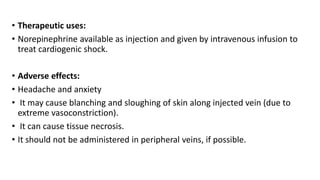
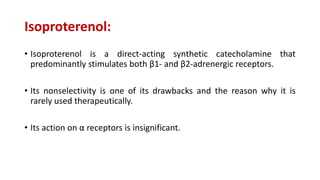
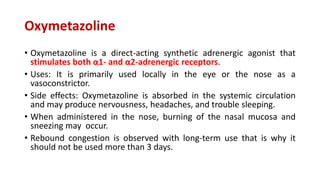
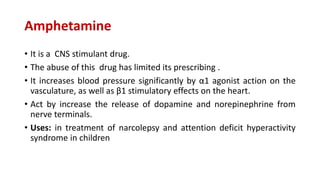
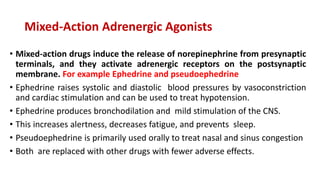
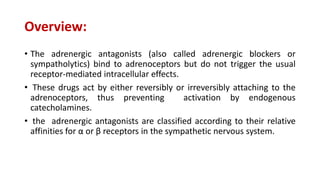
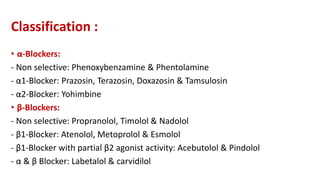
The document discusses the adrenergic system and adrenergic drugs. It describes how adrenergic drugs act on adrenergic receptors stimulated by norepinephrine or epinephrine. It discusses the different types of adrenergic receptors (α and β) and their subtypes, as well as the mechanisms and effects of various adrenergic drugs including epinephrine, norepinephrine, isoproterenol, and oxymetazoline. Key therapeutic uses and side effects are provided for some of the major adrenergic drugs.
![Norepinephrine
• When norepinephrine is given in therapeutic doses to humans, the α-
adrenergic receptor is most affected.
• Cardiovascular actions :
• NE induced vasoconstriction and this causes a rise in peripheral resistance
due to intense vasoconstriction of most vascular beds, including the kidney
(α1 effect) and increase both systolic and diastolic blood pressures .
• Norepinephrine causes greater vasoconstriction than does epinephrine,
because it does not induce compensatory vasodilation via β2 receptors on
blood vessels supplying skeletal muscles, etc.
• weak β2 activity of norepinephrine also explains why it is not useful in the
treatment of asthma.]](https://image.slidesharecdn.com/lec8adrenergicsystem1-240309172928-3dcacd9b/85/Lec-8-adrenergic-system-1-pdf-2000245-23-320.jpg)
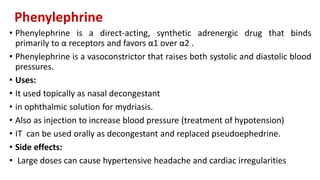

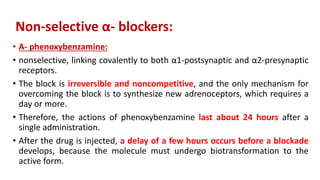
![Cardiovascular effects:
• By blocking α1 receptors, phenoxybenzamine prevents vasoconstriction of
peripheral blood vessels by endogenous catecholamines.
• The decreased peripheral resistance provokes a reflex tachycardia,
arrhythmia, and even ischemic cardiac events.
• The ability to block presynaptic inhibitory α2 receptors in the heart can
contribute to an increased cardiac output. [Note: These receptors when
blocked will result in more norepinephrine release, which stimulates β1
receptors on the heart to increase cardiac output].
• Thus, the drug has been unsuccessful in maintaining lowered blood pressure
in hypertension.](https://image.slidesharecdn.com/lec8adrenergicsystem1-240309172928-3dcacd9b/85/Lec-8-adrenergic-system-1-pdf-2000245-39-320.jpg)