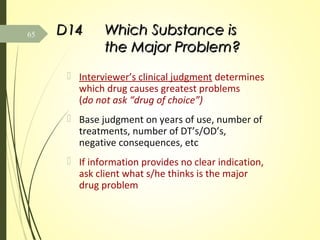
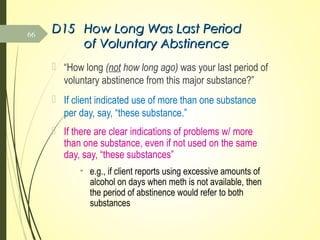
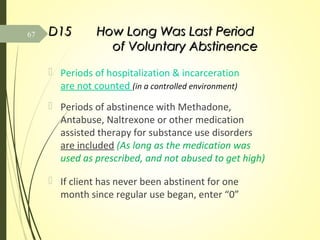
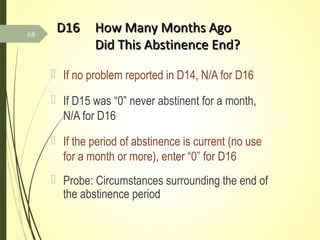
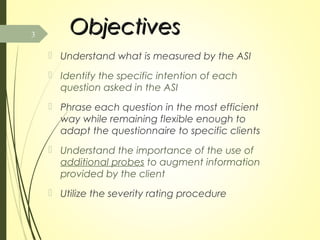
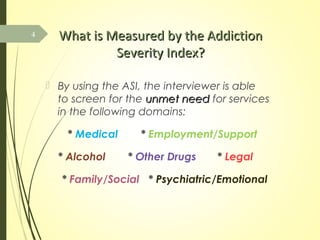
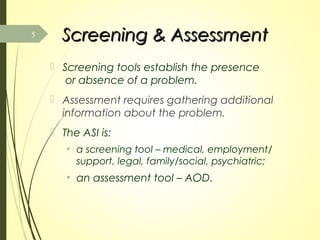
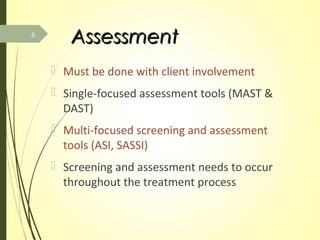
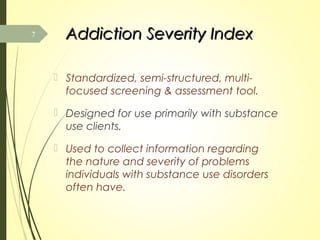
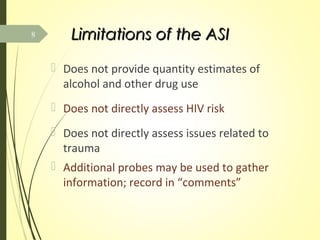
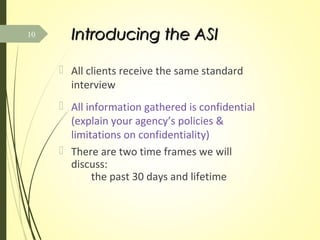
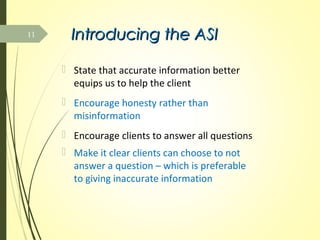
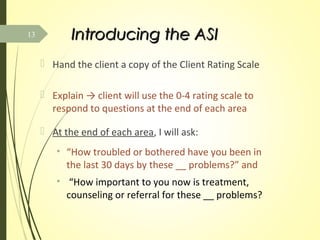
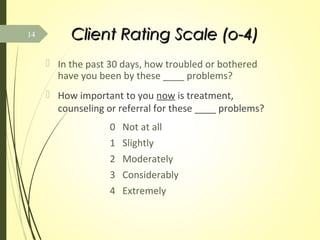
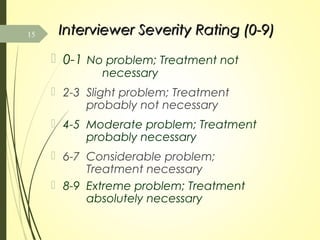
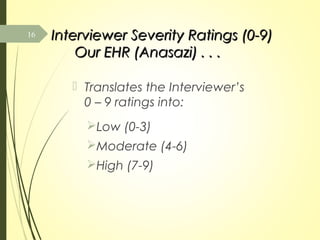
The document provides an introduction and overview for a training on administering the Addiction Severity Index (ASI). It discusses the goal of understanding how to properly use the ASI to screen for problems in various domains. The training covers objectives like understanding what each question measures, how to phrase questions, and how to use additional probes. It also explains how to rate client responses using the ASI's severity scales to determine needed treatment.

![M2 Length of Time SinceM2 Length of Time Since
Last HospitalizationLast Hospitalization
How long ago (not how long) was your last
[overnight] hospitalization?
If occurred within the last month, code 0
years, 1 month. If that hospitalization < 2
weeks, note length of stay in comments
Additional probes: diagnosis/reasons for
hospitalization; types of medications
received
32](https://image.slidesharecdn.com/addictionseverityindexintrotrainingjan2015-150826221747-lva1-app6891/85/Addiction-severity-index-intro-training-jan-2015-32-320.jpg)