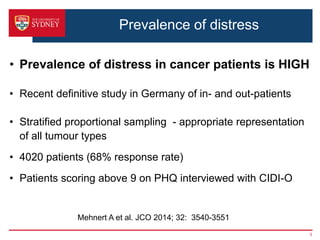
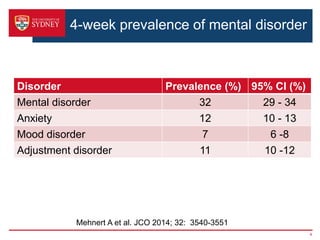
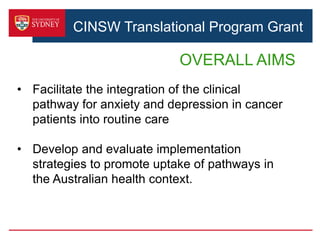
1. This document discusses implementing a clinical pathway for screening and managing anxiety and depression in cancer patients. It outlines barriers to implementation and strategies to address them.
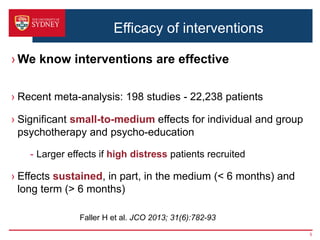
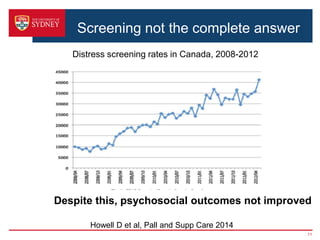
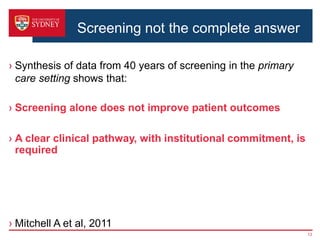
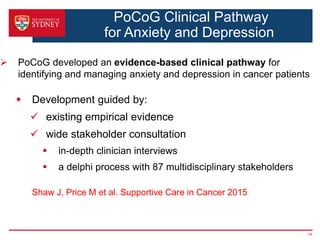
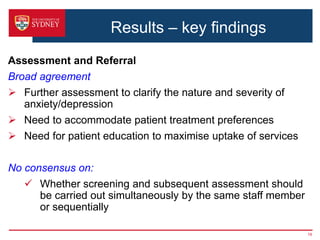
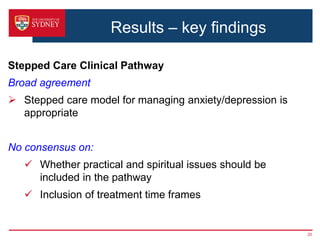
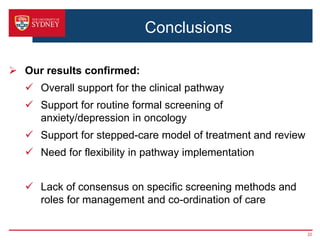
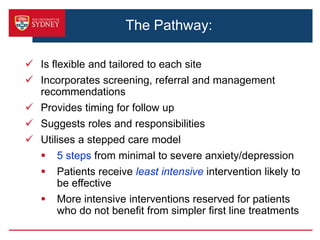
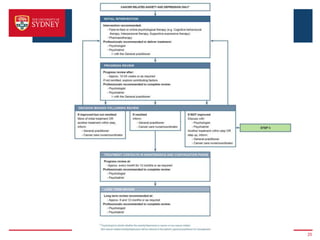
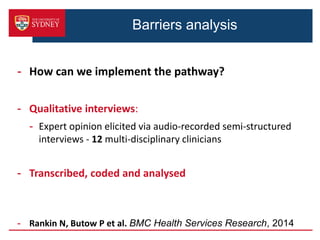
2. A key barrier is that screening alone does not improve outcomes; a clear clinical pathway and institutional support are needed. The pathway was developed through stakeholder consultation and specifies screening, assessment, referral, and treatment steps.
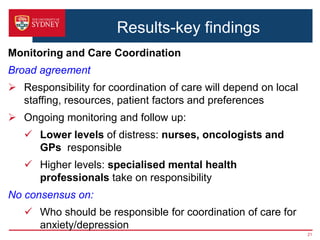
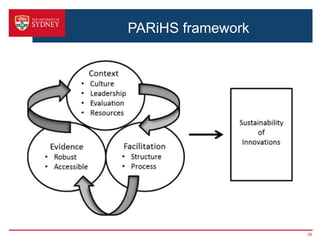
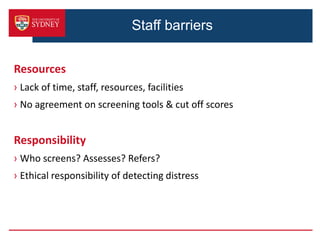
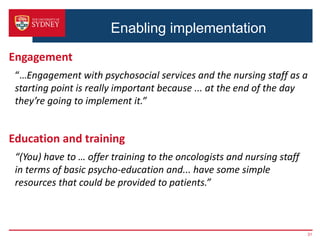
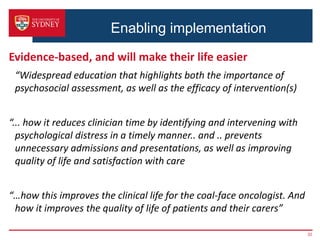
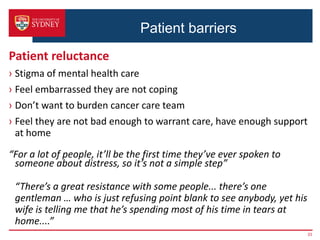
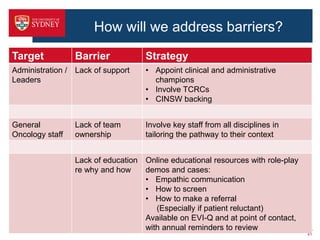
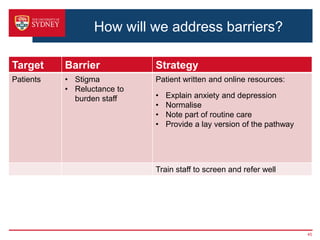
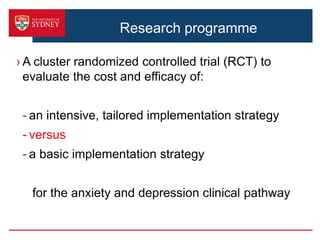
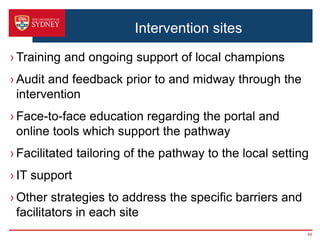
3. Barriers to implementing the pathway include lack of resources, responsibility issues, staff and patient reluctance. The proposed study will test intensive versus basic strategies to promote pathway uptake, including online training, automated screening/referral systems, and patient/staff educational resources. The goal is to improve psychosocial outcomes for cancer patients.