acid-base.@..........................ppt
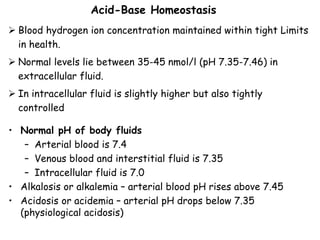
- 1. Blood hydrogen ion concentration maintained within tight Limits in health. Normal levels lie between 35-45 nmol/l (pH 7.35-7.46) in extracellular fluid. In intracellular fluid is slightly higher but also tightly controlled Acid-Base Homeostasis • Normal pH of body fluids – Arterial blood is 7.4 – Venous blood and interstitial fluid is 7.35 – Intracellular fluid is 7.0 • Alkalosis or alkalemia – arterial blood pH rises above 7.45 • Acidosis or acidemia – arterial pH drops below 7.35 (physiological acidosis)
- 2. 2
- 3. Sources of Hydrogen Ions Most hydrogen ions originate from cellular metabolism • Breakdown of sulpher-containing proteins releases H into the ECF • Incomplete oxidation of energy substrates generates acids like: • Anaerobic respiration of glucose produces lactic acid • Fat metabolism yields organic acids and ketone bodies, these intermediates will be further metabolized and consumed (e.g., lactate in gluconeogenesis, oxidation of ketones). • Temporary imbalances between the rates of production and consumption may occur in health (e.g., the accumulation of lactic acid during anaerobic exercise), Transporting carbon dioxide as bicarbonate releases hydrogen ions In disease states, increased hydrogen ion production is an important cause of acidosis. The total amount of hydrogen ion produced each day is 100000 times more acid than normal ! This just does not happen because excess hydrogen ions are efficiently excreted in urine.
- 5. Hydrogen Ion Regulation • Concentration of hydrogen ions is regulated sequentially by: – Chemical buffer systems – act within seconds – The respiratory center in the brain stem – acts within 1-3 minutes – Renal mechanisms – require hours to days to effect pH changes Chemical Buffer Systems • Three major chemical buffer systems – Bicarbonate buffer system – Phosphate buffer system – Protein buffer system Any drift in pH is resisted by the entire chemical buffering system
- 6. Buffering of hydrogen ions As hydrogen ions are generated they are buffered, thus limiting the rise in hydrogen ion concentration which would otherwise occur. A buffer is a solution of the salt or a weak acid which is able to bind hydrogen ions. If hydrogen ions are added to a buffer, some will combine with the conjugate base and convert it to the un-dissociated acid. Buffering does not remove hydrogen ions from the body. Buffers temporarily wash up any excess hydrogen ions which are produced. In the same way that a sponge soaks up water. Buffering is only a short term solution to the problem of excess hydrogen ion. Eventually, the body must get rid of the hydrogen ions by renal excretion. The efficacy of any buffer is limited by its concentration and by the position of the equilibrium
- 7. The body contains Three major chemical buffer systems to resist sudden changes in hydrogen ion production Phosphate buffer system: Phosphate is a minor buffer in the ECF but is of fundamental importance in the urine. Protein buffer system: hemoglobin in the erythrocytes has a high capacity for binding hydrogen ion Bicarbonate buffer system: it is the most important in the ECF Bicarbonate (HCO3 -) combines with hydrogen ion to form carbonic acid (H2CO3) The addition of hydrogen ions increasing the amount of carbonic acid and consuming bicarbonate ions. Conversely, if the hydrogen ion concentration falls, carbonic acid dissociates, thereby generating hydrogen ions. This buffer system is unique in that the H2CO3, can dissociate to water and carbon dioxide. H + HCO H CO + 3 2 3 - 2 2 3 2 CO O H CO H
- 8. Bicarbonate Buffer System • A mixture of carbonic acid (H2CO3) and its salt, sodium bicarbonate (NaHCO3) (potassium or magnesium bicarbonates work as well) • If strong acid is added: – Hydrogen ions released combine with the bicarbonate ions and form carbonic acid (a weak acid) – The pH of the solution decreases only slightly • If strong base is added: – It reacts with the carbonic acid to form sodium bicarbonate (a weak base) – The pH of the solution rises only slightly • This system is the most important ECF buffer
- 9. Simple buffers rapidly become ineffective as the association of the hydrogen ion and the anion of the weak acid reaches equilibrium. The bicarbonate system keeps working because the carbonic acid is removed as CO2. The limit to the effectiveness the bicarbonate system is the initial concentration of bicarbonate. Only when all the bicarbonate is used up does the system have no further buffering capacity. The capacity of the bicarbonate system in the body is greatly enhanced by the fact that carbonic acid can readily be formed from carbon dioxide or disposed of by conversion into carbon dioxide and water. Buffering by the bicarbonate system effectively removes hydrogen ion from the ECF at the expense of bicarbonate. The extracellular fluid contains a large amount of bicarbonate but it falls as H+ is increased To maintain the capacity of the buffer system, the bicarbonate must be regenerated.
- 10. Bicarbonate reabsorption and hydrogen ion excretion The glomerular filtrate contains the same concentration of bicarbonate ions as the plasma If not reabsorbed large amounts would be excreted in the urine depleting the body’s buffering capacity causing an acidosis Virtually all the filtered bicarbonate is reabsorbed. The luminal surface of renal tubular cells is impermeable to bicarbonate and therefore direct reabsorption can not occur. Bicarbonate is reabsorbed indirectly: within the renal tubular cells, carbonic acid is formed from carbon dioxide and water This reaction is catalyzed in the kidney by the enzyme carbonic anhydrase. The carbonic acid thus formed dissociates to give hydrogen and bicarbonate ions. The bicarbonate ions pass across the basal border of the cells into the interstitial fluid. The hydrogen ions are secreted across the luminal membrane in exchange for sodium ions, which accompany bicarbonate into the interstitial fluid.
- 13. Hydrogen ion excretion Although hydrogen ions are secreted into the tubular fluid, there is no net hydrogen ion excretion, as the formation of hydrogen ions provides the means for the reabsorption of bicarbonate. Hydrogen ion excretion depends upon the same reactions occurring in the renal tubular cells but, in addition, requires the presence of a suitable buffer system in the urine The excreted hydrogen ions must be buffered in urine or the [H+] would rise to very high levels. Phosphate acts as one such buffer, while ammonia is another.
- 14. Bicarbonate reabsorption and hydrogen ion excretion The principal urinary buffer is phosphate. This is present in the glomerular filtrate (HPO42-). This combines with hydrogen ions and is converted to H2PO4-. Ammnia, produced by the deamination of glutamine by glutaminase enzyme in renal tubular cells, Ammonia can readily diffuse across cell membranes and ammonium ions are formed and excreted. HPO + H H PO 4 + 2 4 - 2- NH H NH 3 4
- 15. Bicarbonate generation and hydrogen ion excretion
- 16. Transport of Carbon dioxide Carbon dioxide, produced by aerobic metabolism, diffuses out of cells and dissolves in the ECF. A small amount combines with water to form carbonic acid, thereby increasing the hydrogen ion concentration of the ECF. In red blood cells, metabolism is anaerobic and little carbon dioxide is produced. Carbon dioxide thus diffuses into red cells down a gradient and carbonic acid is formed, facilitated by carbonate dehydatase (Carbonic unhydrase) The overall effect of this process is that carbon dioxide is converted to bicarbonate in red blood cells. This bicarbonate diffuses out of the red cells with exchange with chloride ions (the chloride shift). In the lungs, the reverse process occurs because of the low partial pressure of carbon dioxide in the alveolar capillaries. Carbon dioxide is produced from bicarbonate and diffuses into the alveoli to be excreted in the expired air.
- 17. How is CO2 Exported? Most of the carbon dioxide in the blood is present in the form of bicarbonate. Dissolved carbon dioxide, carbonic acid and carbamino compounds (compounds of carbon dioxide and protein) account for less than 2.0 mmol/L in a total carbon dioxide con. of appro. 26 mmol/L. The term ‘bicarbonate’ and ‘total carbon dioxide’ are frequently used synonymously.
- 18. Assessing Acid-base Status An indication of the acid-base status of the patient can be obtained by measuring the components of the bicarbonate buffer system. 2 2 3 2 CO O H CO H H + HCO H CO + 3 2 3 - - 3 2 + HCO PCO to l proportina is H Excess hydrogen ions are buffered by bicarbonate the formed carbonic acid dissociates carbon dioxide is lost in the expired air limits the potential rise in hydrogen ion concentration at the expense of a reduction in bicarbonate The hydrogen ion concentration in blood varies as the bicarbonate concentration and PCO2 change. If everything else remains constant: Adding hydrogen ion, removing bicarbonate or increasing the PCO2 will all have the same effect an increase in [H+]. Removing hydrogen ions, adding bicarbonate or lowering PCO2 will all cause the [H+] to fail. Blood [H+] is 40 nmol/l and is controlled by our normal pattern of respiration and the functioning of our kidneys.
- 20. When you see “respiratory”, think PCO2 When you see “metabolic”, think [HCO3] 20 Remember Disorders of hydrogen ion homeostasis “Metabolic” acid-base disorders are those that directly cause a change in the bicarbonate concentration, like diabetes mellitus because of the absence of insulin building up of [H+], of ketone bodies or loss or bicarbonate from the extracellular fluid. “Respiratory” acid-base disorders affect PCO2. Impaired respiratory function causes a build up of CO2 in blood or in the case of hyperventilation causes a decreased PCO2
- 21. Compensation The body has physiological mechanisms which try to restore [H+] to normal. These processes are called 'compensation', The observed [H+] in any acid-base disorder reflects the balance between the primary disturbance and the amount of compensation. Renal Compensation: where lung function is compromised (primary respiratory disorder). The body attempts to increase the excretion of hydrogen ion via the renal route. Renal compensation is slow to lake place. Respiratory compensation: where there are metabolic disorder some compensation is possible by lung
- 22. Disorders of hydrogen ion homeostasis Acidosis and alkalosis are clinical terms which define the primary acid-base disturbance. They can be used even when the [H+] is within the normal range. i.e. when the disorders are fully compensated. The definitions are: Non-respiratory (Metabolic) acidosis: The primary disorder is a decrease in bicarbonate concentration. Non-respiratory (Metabolic) alkalosis: The primary disorder is an increased bicarbonate. Respiratory acidosis: The primary disorder is an increased PCO2. Respiratory alkalosis: The primary disorder is a decreased PCO2. Primary mixed acid-base disorders, that is, disorders of combined respiratory and non-respiratory origin, ‘Acidemai' and 'alkalaemia' refer simply to whether the [H+] in blood is higher or lower than normal
- 23. metabolic acidosis The primary abnormality in non-respiratory acidosis is either increased production or decreased excretion of hydrogen ions. In some cases, both of these may contribute. Loss of bicarbonate and retention of hydrogen ions may result in acidosis in patients losing alkaline secretions from the small intestine. Causes of non-respiratory acidosis * Increased H+ formation ketoacidosis (usually diabetic, also alcoholic) lactic acidosis poisoning: e.g., ethanol, methanol, ethylene glycol and salicylate * Acid ingestion acid poisoning * Decreased H+ excretion renal tubular acidosis generalised renal failure carbonate dehydratase inhibitors * Loss of bicarbonate diarrhea pancreatic, intestinal and biliary fistulae or drainage
- 25. The characteristic biochemical changes seen in the blood in non-respiratory acidosi can be summarized as follows: metabolic acidosis high [H+], Low pH, low PCO2 and Low [HCO3 -] Compensation is effected by hyperventilation, which increases the removal of carbon dioxide and lowers the PCO2. Hyperventilation is a direct result of the increased [H+] stimulating the respiratory centre. Respiratory compensation cannot completely normalize the [H+] since it is the high concentration itself that stimulates the compensatory hyperventilation. Also the increased work of the respiratory muscle produces carbon dioxide, so limiting the extent to which the pCO2 can be lowered. In a healthy person, hyperventilation would produce a respiratory alkalosis. If renal function is normal in a patient with non-respiratory acidosis, excess hydrogen ions can be excreted by the kidneys. The complete correction of a metabolic acidosis requires reversal of the underlying cause, for example, rehydration and insulin for diabetic ketoacidosis. Hyperkalaemia is common in acidotic patients.
- 26. Clinical effects of acidosis The compensatory response to metabolic acidosis is hyperventilation, since the increased [H+] acts as a powerful stimulant of the respiratory centre. The deep, rapid and gasping respiratory pattern is known as Kussmaul breathing. Hyperventilation is the appropriate physiological response to acidosis and it occurs rapidly. A raised [H+] leads to increased neuromuscular irritability. There is a hazard of arrhythmias progressing to cardiac arrest, this will be more likely in the presence of hyperkalaemia which will accompany the acidosis Depression of consciousness can progress to coma and death.
- 27. • Total concentration of anions and cations in plasma must be equal to maintain electrical neutrality • but, only certain cation (Na+ with or without K +) and anions (Cl-, HCO3 -) are routinely measured in clinical laboratory Anion Gap
- 28. • “anion gap” : difference between unmeasured anions and unmeasured cations Na+ unmeasured cations unmeasured anions Cl- HCO3 - Anion Gap
- 29. • anion gap = [Na+] – {[HCO3 -] + [Cl-]} = 144 - { 24 + 108} = 10 mEq/L Na+ unmeasured cations unmeasured anions Cl- HCO3 - Anion Gap
- 30. • if unmeasured anions relative amount of Cl- & HCO3 - • anion gap • if unmeasured cation relative amount of Na+ Na+ unmeasured cations unmeasured anions Cl- HCO3 - albumin, phosphate, sulfate, other organic anions calcium, magnesium, potassium Anion Gap
- 31. • In metabolic acidosis (low HCO3 -) • if plasma Na+ is unchanged, • concentration of anions (Cl- or unmeasured anion) must increase to maintain electro- neutrality (1) if Cl- remains unchanged: • there must be increased unmeasured anion (= anion gap) a. diabetes mellitus (ketoacidosis) b. lactic acidosis c. chronic renal failure d. aspirin (acetylsalicylic acid) e. methanol f. ethylene glycol0 Clinical Use of anion gap
- 32. (2) if Cl- increases in proportion to the fall of HCO3 -: • (normal anion gap) • (“hyperchloremic metabolic acidosis) a. diarrhea b. renal tubular acidosis Clinical Use of anion gap
- 33. Metabolic Alkalosis (Non-respiratory alkalosis): is characterized by a primary increase in the ECF bicarbonate concentration, with a consequent reduction in [H+]. Normally, an increase in plasma bicarbonate concentration leads to incomplete renal tubular bicarbonate reabsorption and excretion of bicarbonate in the urine. BUT in Metabolic alkalosis, high renal bicarbonate reabsorption occurs. Factors which may be responsible for this include a decrease in ECF volume, mineralocorticoid excess increased Sod along with carbonate reabsorption and potassium depletion. Massive quantities of bicarbonate must be ingested to produce a sustained alkalosis.
- 34. Metabolic Alkalosis (Non-respiratory alkalosis): The causes of a metabolic alkalosis are: Loss of Hydrogen ion in gastric fluid during vomiting especially when there is no parallel loss of bicarbonate. Ingestion of an absorbable alkali as sod bicarbonate: very large quantities are required except there is renal impairment In sever potassium depletion (consequences of diuretic therapy) hydrogen ions are retained inside cells to replace missing potassium ions. In renal tubules more hydrogen are exchanged for reabsorption of sod. So, despite there being an alkalosis, the patient passes acidic urine. This often referred to as a ‘paradoxical’ acid urine, because in other causes of metabolic alkalosis urinary [H+] usually falls.
- 36. Clinical effects of metabolic alkalosis The clinical effects of alkalosis include: hypoventilation, confusion and eventually coma. Muscle cramps, tetany and paraesthesia (any abnormality in sensation) may be a consequence of a decrease in the unbound plasma calcium concentration which is a consequence of the alkalosis.
- 37. Metabolic Alkalosis (Non-respiratory alkalosis): The correction of non-respiratory alkalosis requires reversal both of the primary cause and for the mechanism for its maintenance. The expected compensatory would be an increased in PCO2 which would increase the ratio PCO2/[HCO3] and thus [H+]. A low arterial [H+] inhibits the respiratory centre, causing hypoventilation, and thus an increase in PCO2. However, since an increase in PCO2 is itself a powerful stimulus to respiration, this compensation, particularly in acute non-respiratory alkalosis, may be self-limiting. In more chronic disorders, significant compensation may occur, presumably because the respiratory centre becomes less sensitive to carbon dioxide. Should hypoventilation lead to significant hypoxaemia, however, this will provide a powerful stimulus to respiration and prevent further compensation.
- 38. Management: The management of a non-respiratory alkalosis depends upon the severity of the condition and upon the cause. When hypovolaemia are present, they can be simultaneously corrected by an infusion of isotonic sodium chloride solution (normal saline) which will also improve renal perfusion and allow excretion of the bicarbonate load. It is very rarely necessary to attempt rapid correction of non- respiratory alkalosis, for example, by administration of ammonium chloride. The mild alkalosis commonly associated with potassium depletion may require correction
- 39. Respiratory acidosis: The primary disorder is an increased PCO2 Respiratory acidosis is characterized by an increase in PCO2, (CO2 retention) For every hydrogen ion produced a bicarbonate ion is generated BUT the effect of adding one H+ to a concentration of 40 nmol/l is much greater than adding one bicarbonate molecule to a concentration of 26 mmol/l. The majority of hydrogen ions are buffered by intracellular buffers, particularly hemoglobin.
- 40. Respiratory acidosis: The primary disorder is an increased PCO2 Respiratory acidosis: Respiratory acidosis may be acute or chronic. Acute conditions occur within minutes or hours, they are uncompensated. Renal compensation has no time to develop as the mechanisms that adjust bicarbonate reabsorption take 48-72 hours to become fully effective. The primary problem in acute respiratory acidosis is alveolar hypoventilation If airflow is completely or partially reduced, the PCO2 in the blood will rise immediately and the [H+] will rise quickly. A resulting low PO2 and high PCO2 causes coma. If this is not relieved rapidly, death results. Examples of acute respiratory acidosis are: Acute airway obstruction: choking (obstruction of the flow of air from the environment into the lungs), bronchopneumonia, acute exacerbation of asthma. Depression of respiratory centre: Anaesthetics, Sedatives
- 41. Chronic respiratory acidosis: usually results from chronic obstructive airways disease (COAD) and is usually a long- standing condition, accompanied by maximal renal compensation. In a chronic respiratory acidosis the primary problem is also usually impaired alveolar ventilation, but renal compensation contributes markedly to the acid-base picture. Compensation may be partial or complete. The kidney increases hydrogen ion excretion and ECF bicarbonate levels rise. Blood [H+] tends back towards normal
- 42. Management of Acidosis The aim when treating respiratory acidosis is to improve alveolar ventilation and lower the PCO2. In acute alveolar hypoventilation: hypoxia causes the main threat to life If ventilation is stopped abruptly, death from hypoxia will occur In chronic respiratory acidosis, it is rarely possible to correct the underlying cause and treatment is directed at maximizing alveolar ventilation by, for example, utilizing physiotherapy, bronchodilators and antibiotics.
- 43. Respiratory alkalosis Respiratory alkalosis is much less common than acidosis but can occur when respiration is stimulated or is no longer subject to feedback control. Usually these are acute conditions, and there is no renal compensation. Renal compensation in a respiratory alkalosis develops slowly, as it does in respiratory acidosis. The treatment is to inhibit or remove the cause of the hyperventilation, and the acid-base balance should return to normal. Causes are: hysterical over-breathing, mechanical over- ventilation in an intensive care patient, raised intracranial pressure, or hypoxia, both of which may stimulate the respiratory center.
- 44. Mixed acid-base disorders Patients can have more than one acid-base disorder. A patient may have both a metabolic and respiratory acidosis, such as the chronic bronchitic patient who develops renal impairment the PCO2 will be increased and the bicarbonate concentration will be low, Hyperventilation causing a respiratory alkalosis, with prolonged nasogastric suction that causes a metabolic alkalosis Sometimes the two acid-base conditions are antagonistic in the way they affect the [H+], a metabolic acidosis and a co-existent respiratory alkalosis, Some examples of mixed acid-base disorders commonly encountered are: A patient with chronic obstructive airways disease, causing a respiratory acidosis, with thiazide-induced potassium depletion and consequent metabolic alkalosis Salicylate poisoning in which respiratory alkalosis occurs due to stimulation of the respiratory centre, together with metabolic acidosis due to the effects of the drug on metabolism.
- 45. Interpretation of Acid-Base Data A comprehensive understanding of the pathophysiology of acid-base homoeostasis is essential for the correct interpretation of laboratory data, but these data should always be considered in the clinical background. The starting point in any evaluation should be the hydrogen ion concentration or pH. This will indicate whether the predominant disturbance is an acidosis or an alkalosis. However, a normal value does not exclude an acid-base disorder. There may be either a fully compensated disturbance or Two primary disturbances where effects on hydrogen ion concentration cancel each other out. If the PCO2 is abnormal, there must be a respiratory component to the disturbance; if the PCO2 is raised in an acidosis, the acidosis is respiratory and the value of the hydrogen ion concentration will indicate wither there is an additional metabolic component. If the PCO2 is low in an acidosis, the acidosis is non-respiratory and there is an additional respiratory component, which will often reflect compensation. A similar rationale applies to alkalotic states.
- 46. 46
- 47. Interpretatio n of Acid- Base Data
- 49. 1. Know the clinical details of the patient 2.Find the cause of the acid-base disorder 3.The snapshot problem: Are the results 'current'? 4.Determine the major primary process then select the correct rule. The bedside rules
- 50. Rule 1 : The 1 for 10 Rule for Acute respiratory Acidosis The [HCO3] will increase by 1 mmol/l for every 10 mmHg elevation in pCO2 above 40 mmHg. Expected [HCO3] = 24 + { (Actual pCO2 - 40) / 10 } Rule 2 : The 4 for 10 Rule for Chronic Respiratory Acidosis The [HCO3] will increase by 4 mmol/l for every 10 mmHg elevation in pCO2 above 40mmHg. Expected [HCO3] = 24 + 4 { (Actual pCO2 - 40) / 10} Rule 3 : The 2 for 10 Rule for Acute Respiratory Alkalosis The [HCO3] will decrease by 2 mmol/l for every 10 mmHg decrease in pCO2 below 40 mmHg. Expected [HCO3] = 24 - 2 { ( 40 - Actual pCO2) / 10 } Rules for Respiratory Acid-Base Disorders
- 51. Rules for Respiratory Acid-Base Disorders Rule 4 : The 5 for 10 Rule for a Chronic Respiratory Alkalosis The [HCO3] will decrease by 5 mmol/l for every 10 mmHg decrease in pCO2 below 40 mmHg. Expected [HCO3] = 24 - 5 { ( 40 - Actual pCO2) / 10 } ( range: +/- 2) Rule 5 : The One & a Half plus 8 Rule - for a Metabolic Acidosis The expected pCO2 (in mmHg) is calculated from the following formula: Expected pCO2 = 1.5 x [HCO3] + 8 (range: +/- 2) Rule 6 : The Point Seven plus Twenty Rule - for a Metabolic Alkalosis The expected pCO2(in mmHg) is calculated from the following formula: Expected pCO2 = 0.7 [HCO3] + 20 (range: +/- 5)
- 52. • The history usually strongly suggests the disorder which is present • The net pH change indicates the disorder if only a single primary disorder is present • An elevated anion gap or elevated chloride define the 2 major groups of causes of metabolic acidosis
Editor's Notes
- Intracranial pressure (ICP) is the pressure inside the skull and thus in the brain tissue and cerebrospinal fluid (CSF).