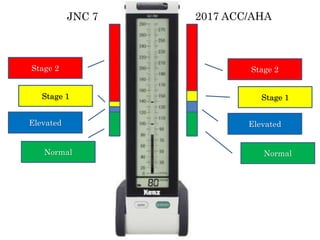
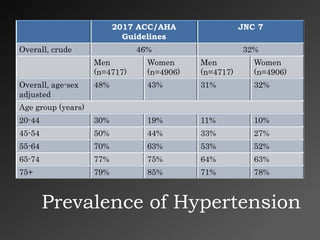
The 2017 ACC/AHA guidelines provide an updated classification of blood pressure levels and recommendations for diagnosing and treating hypertension. Key points include:
1) The guidelines lower the thresholds for elevated blood pressure and define prehypertension as 120-139/80-89 mmHg and stage 1 hypertension as 140-159/90-99 mmHg.
2) Both higher systolic and diastolic blood pressure are associated with increased risk of cardiovascular disease.
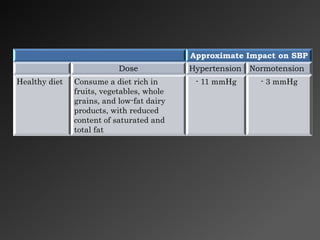
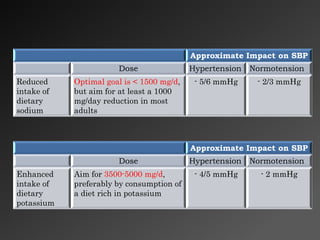
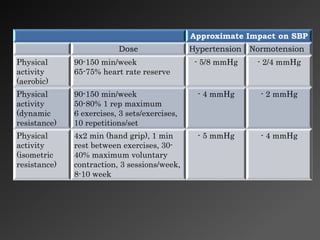
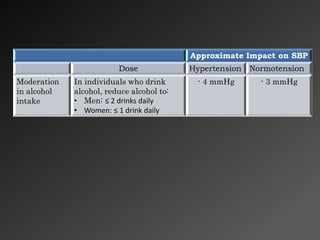
3) Lifestyle modifications like weight loss, reduced sodium intake, and increased physical activity can significantly reduce blood pressure, especially in patients with hypertension.
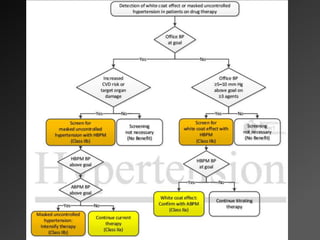
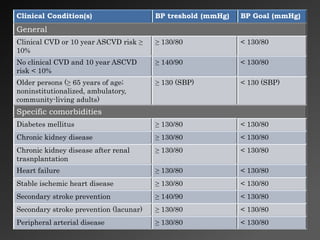
4) Target blood pressure levels for treatment depend on patient risk factors and comorbidities, but