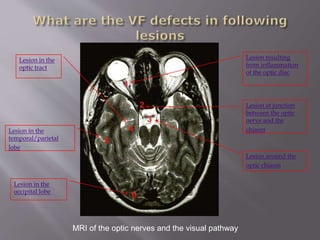
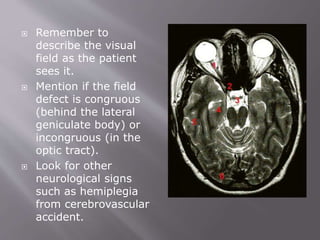
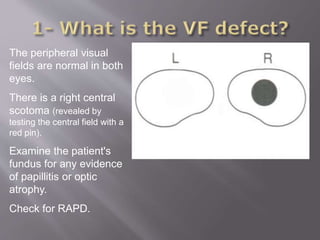
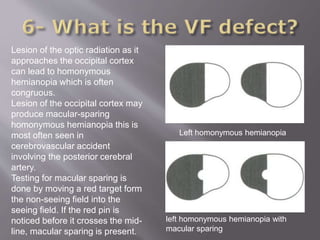
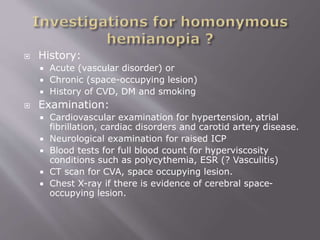
There are several types of visual field defects that can occur based on the underlying condition and location of lesions along the visual pathway. Common visual field defects include tunnel vision, altitudinal defects, and arcuate scotomas. The visual field defects provide clues to the location of lesions in structures like the optic nerves, chiasm, tracts, or occipital lobes. A thorough examination of the eye, visual fields, and neurological evaluation is needed to localize the lesion and identify potential causes.