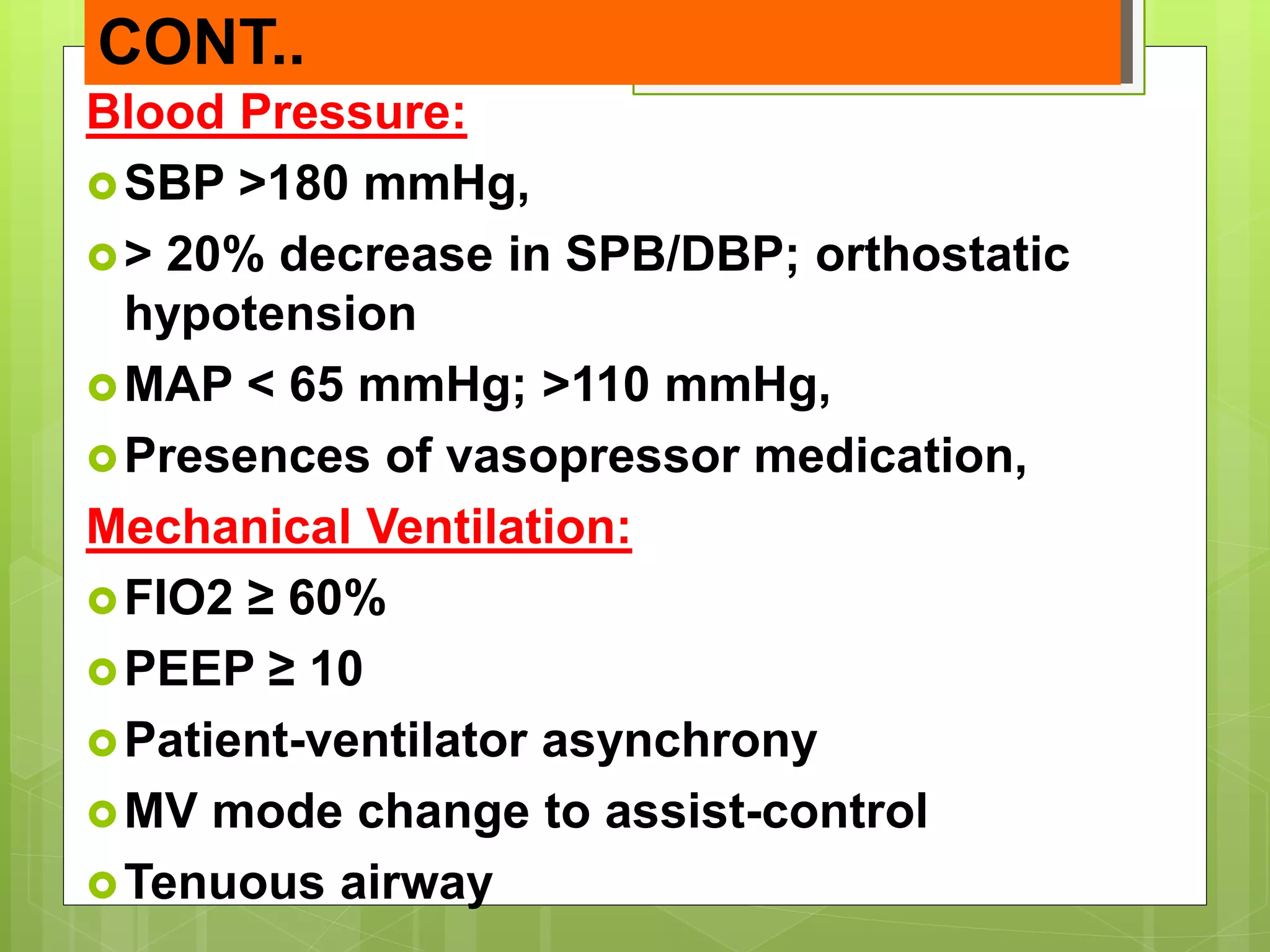
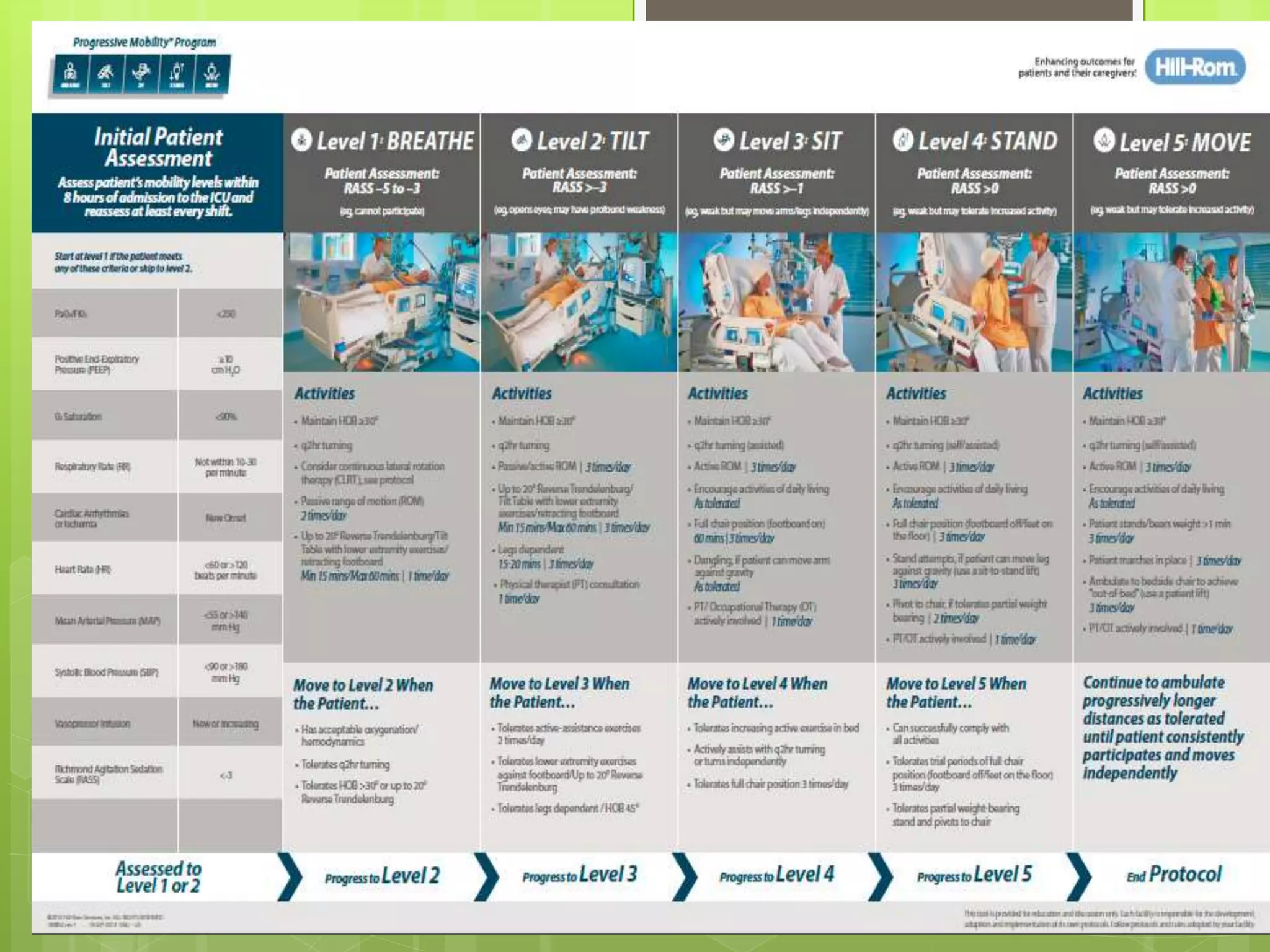
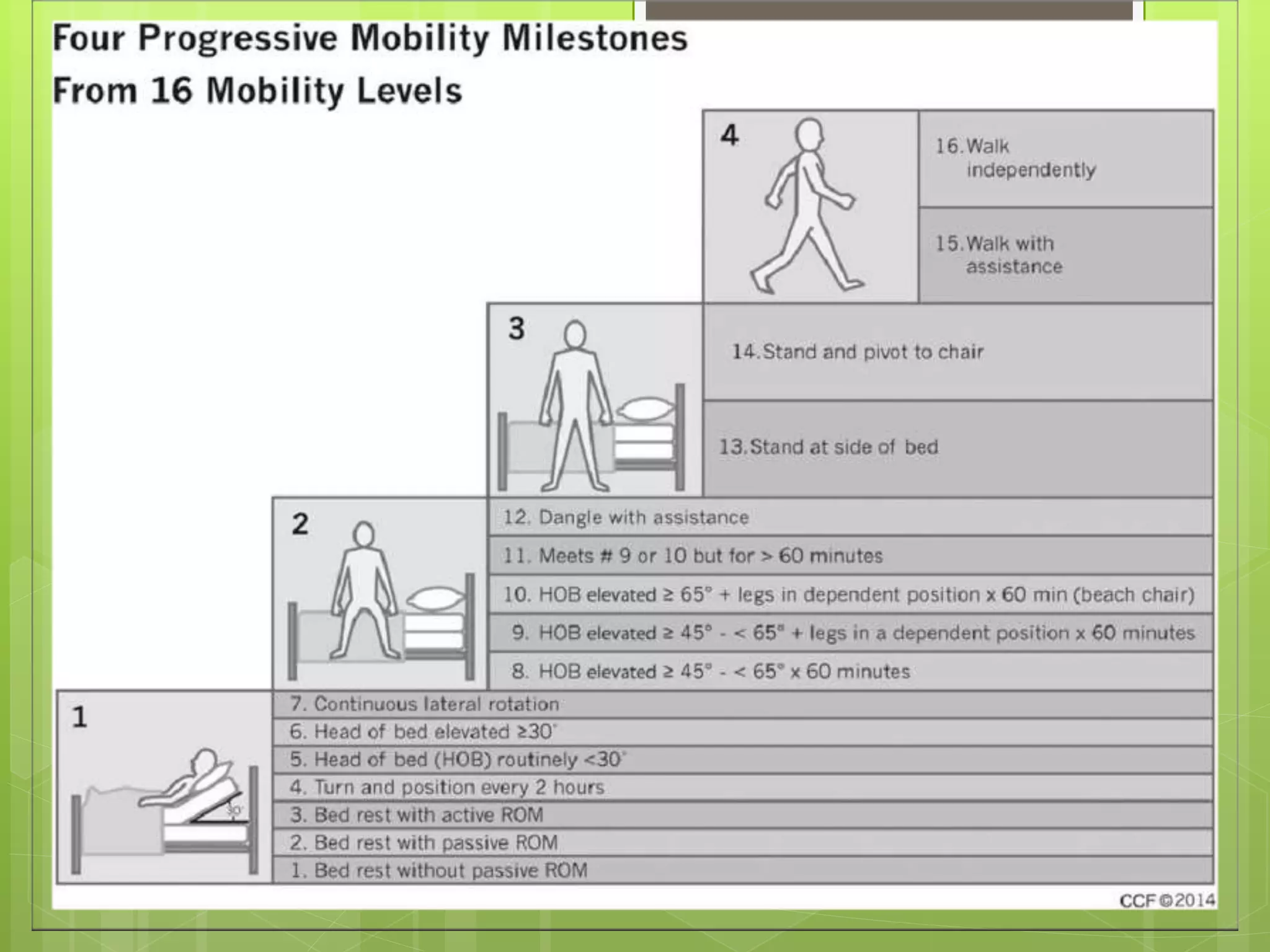
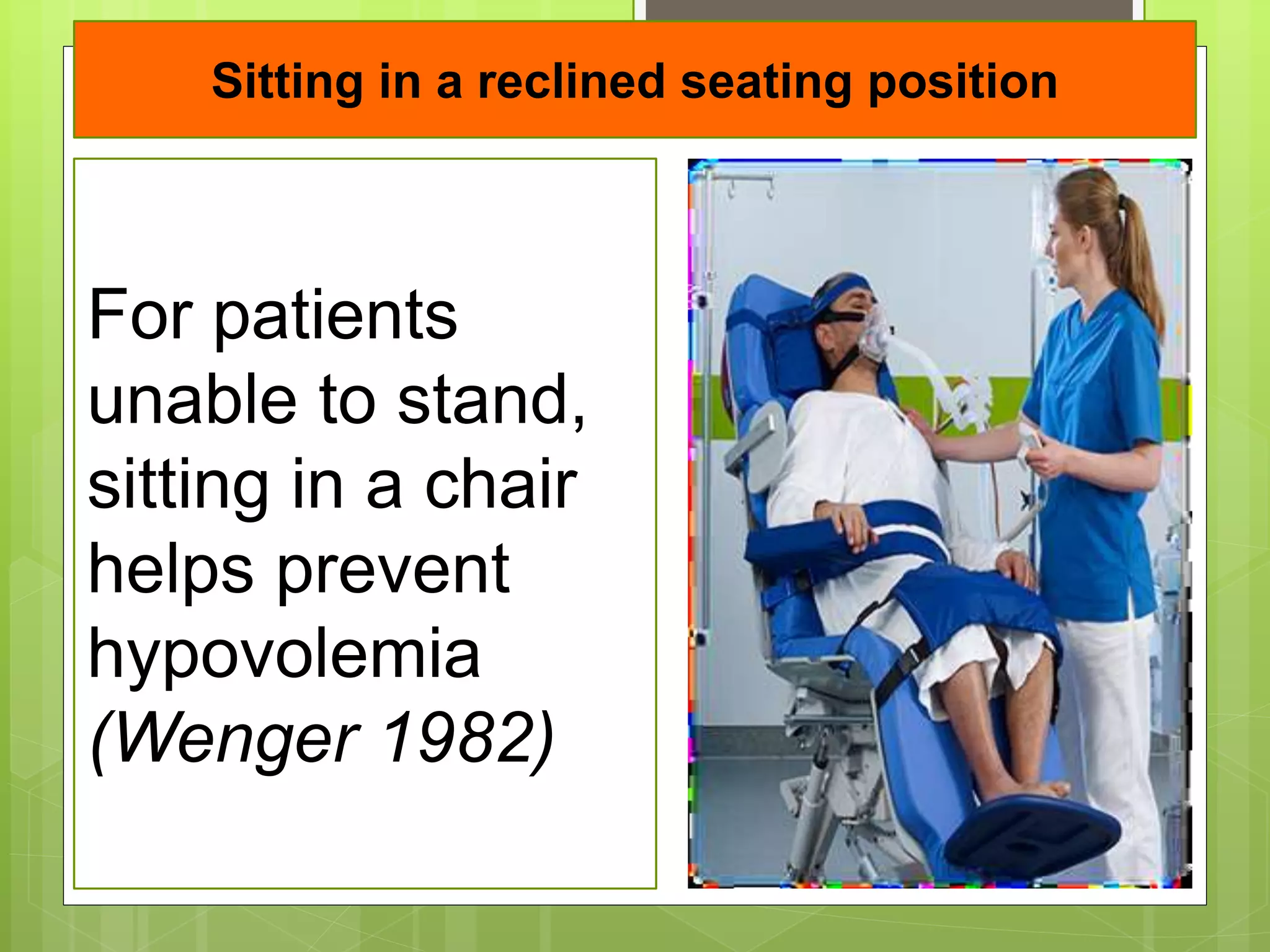
This document presents information on early mobilization for ICU patients. It defines mobilization as physical activity that improves hemodynamic parameters and counters the effects of bed rest. Early mobilization refers to activity within the first 2-5 days of critical illness. The benefits of early mobilization include reduced ICU and hospital stays, faster recovery of respiratory and muscle strength, and lower rates of delirium. The document outlines parameters and safety criteria for passive and active mobilization. Common barriers to early mobilization in the ICU include patient instability, limited staff and equipment, and deep sedation of patients.