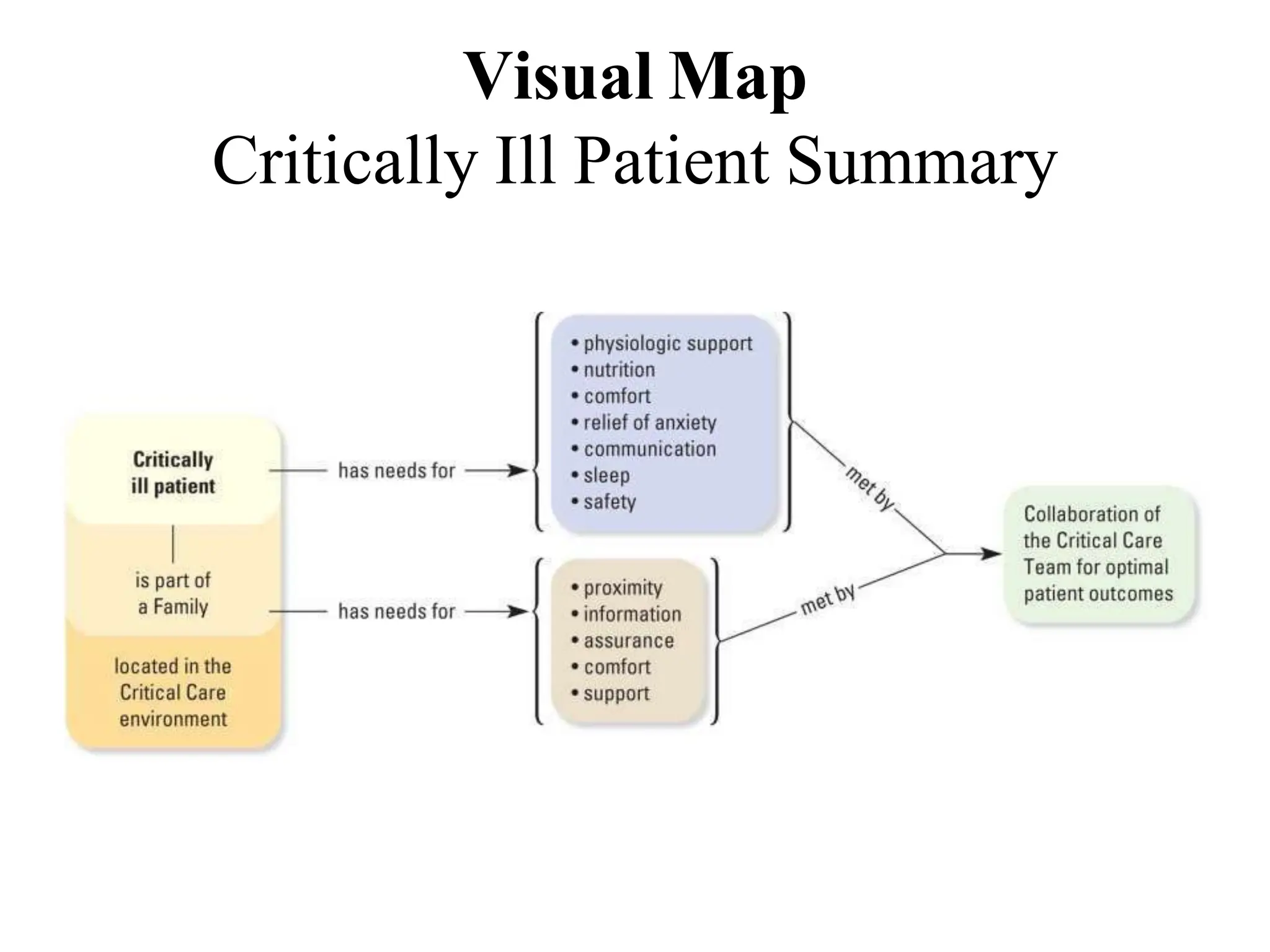
This document outlines the care of critically ill patients in the intensive care unit (ICU). It discusses the levels of care in the ICU from general ward care to intensive care. It describes the comprehensive management of critically ill patients which includes monitoring, respiratory, cardiovascular, gastrointestinal, nutritional, infection control and psychological support. Key aspects of care include pain management, reducing anxiety, preventing complications like delirium, sleep disturbances, and meeting the needs of family members of critically ill patients. The overall aim is to provide optimal care, support rehabilitation and improve the patient and family experience in the ICU.
![CARE OF CRITICALLY ILL
PATIENT:
JOHNY WILBERT, M.Sc[N]
LECTURER,
APOLLO INSTITUTE OF HOSPITAL
MANAGEMENT AND ALLIED SCIENCE](https://image.slidesharecdn.com/careofcriticallyillpatient-180617105854-240401081942-b1166e91/75/careofcriticallyillpatient-180617105854-pptx-1-2048.jpg)