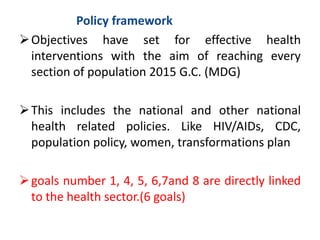
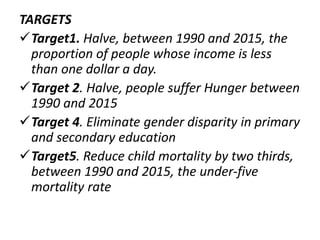
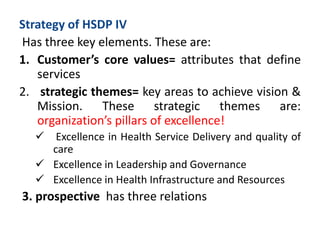
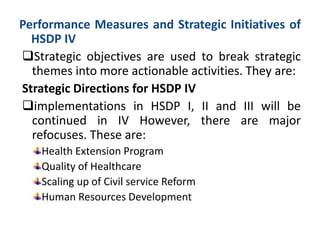
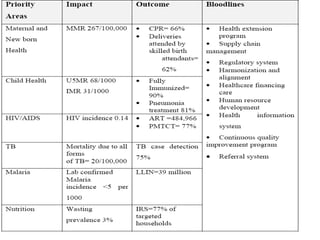
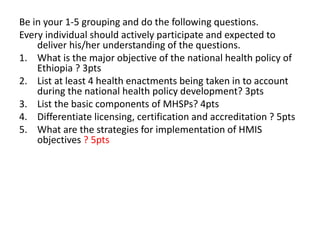
The document outlines the Ethiopian health service program and regulations, detailing the national health policy objectives aimed at equitable health service delivery. It discusses various strategies, programs, and regulations necessary for improving health outcomes, particularly focusing on areas such as maternal and child health, disease control, and health workforce development. Key components include the Health Service Development Program (HSDP) and its phases, which emphasize access, quality, and management of health services in Ethiopia.