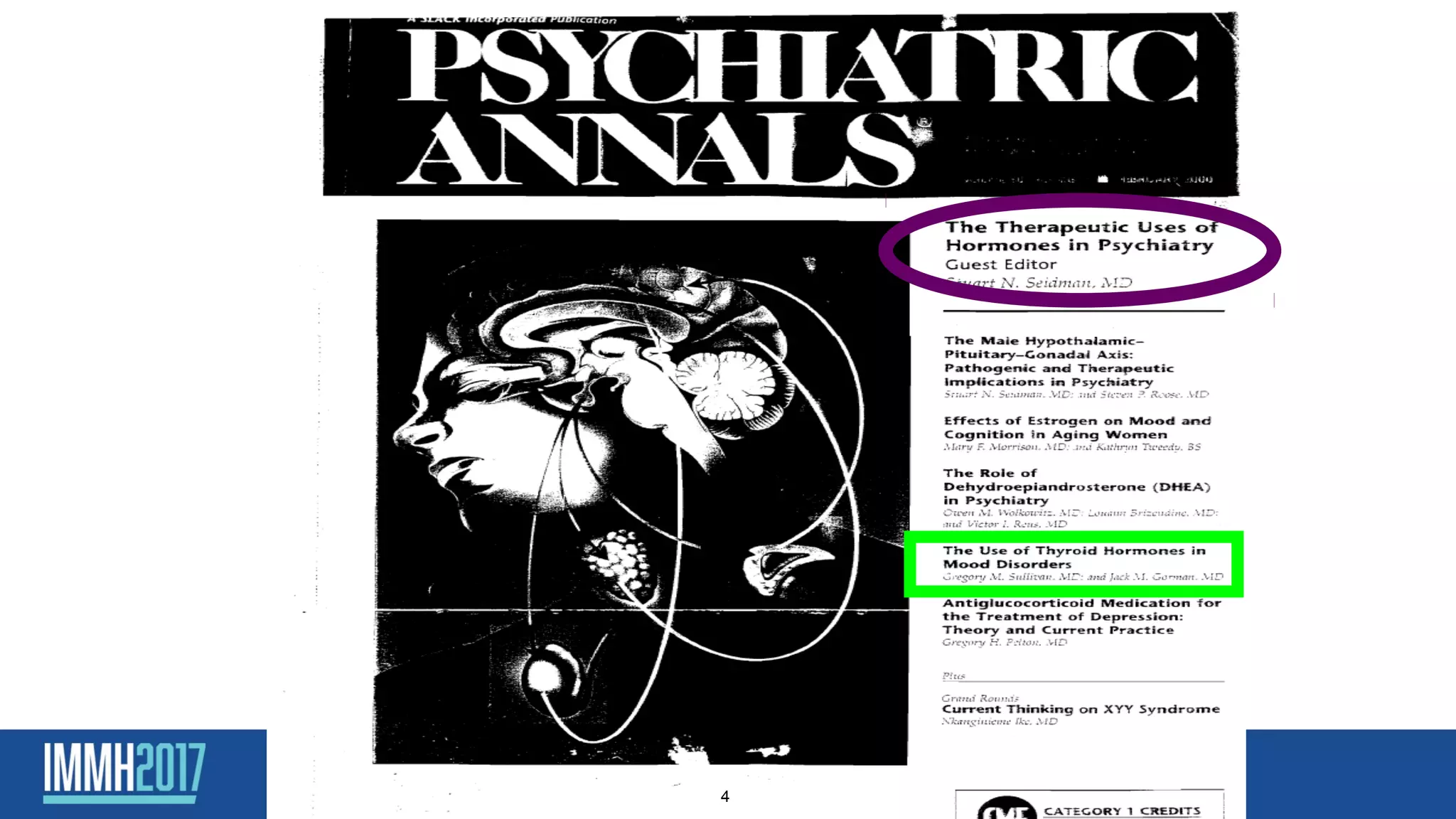
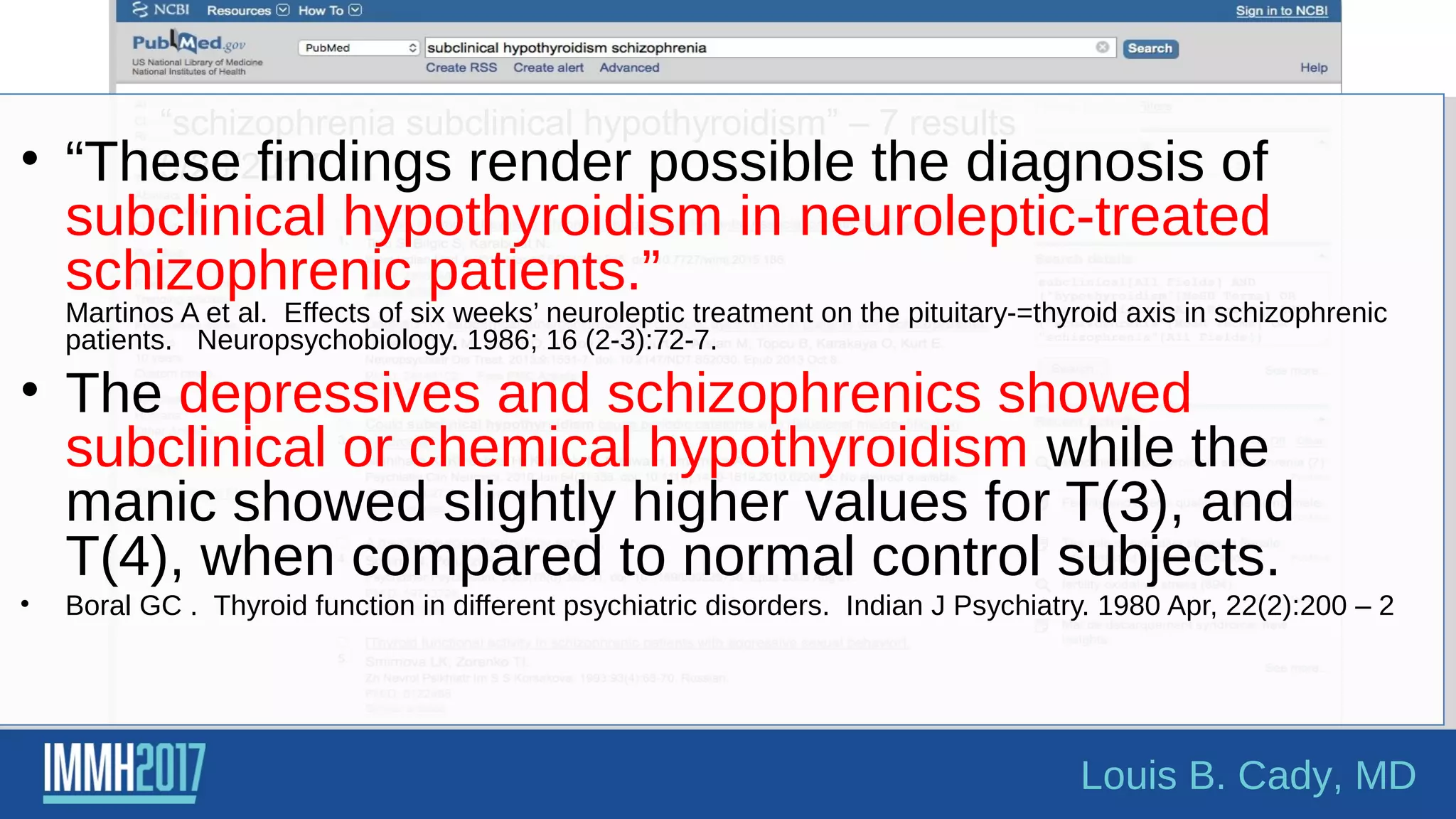
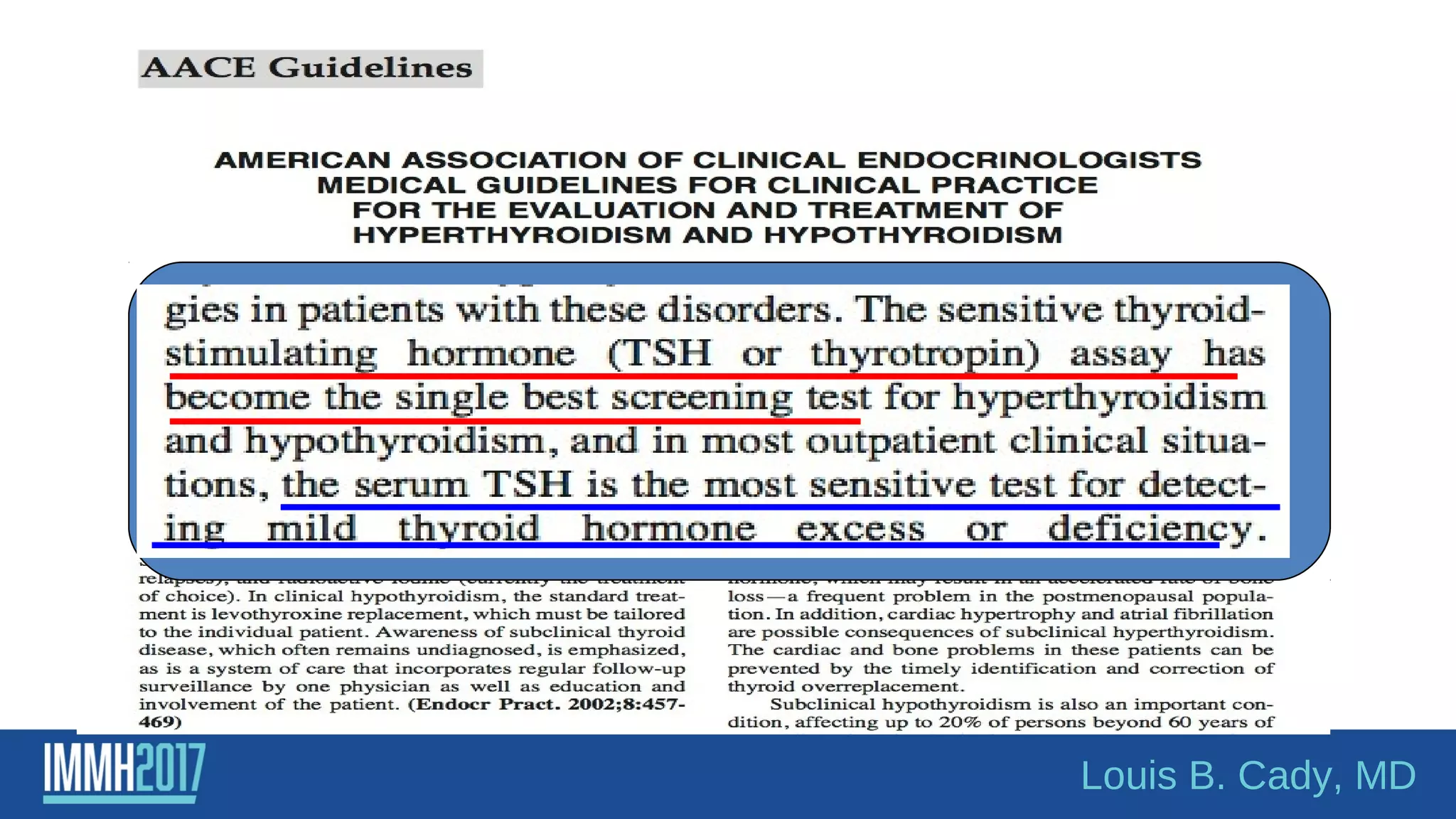
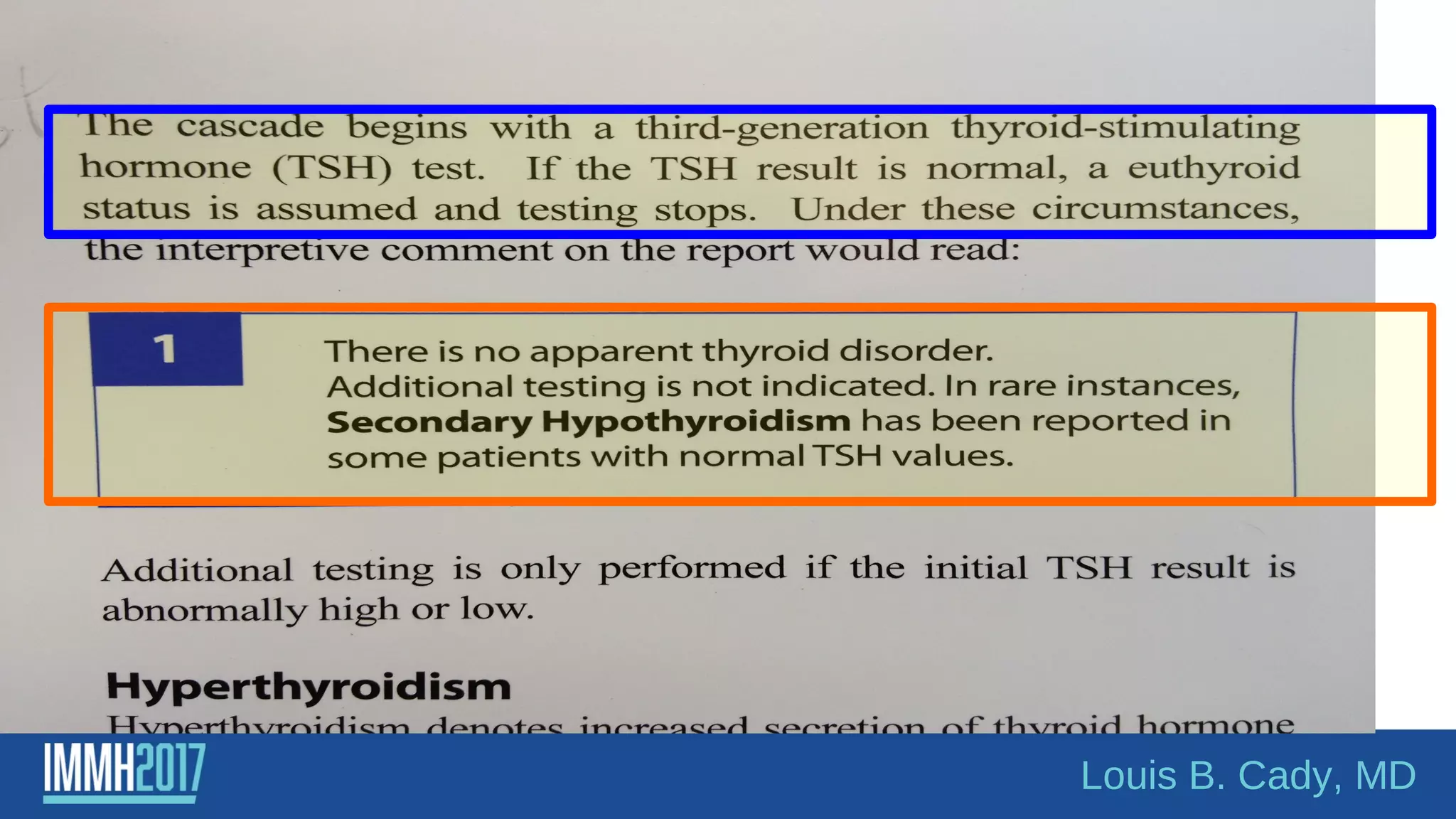
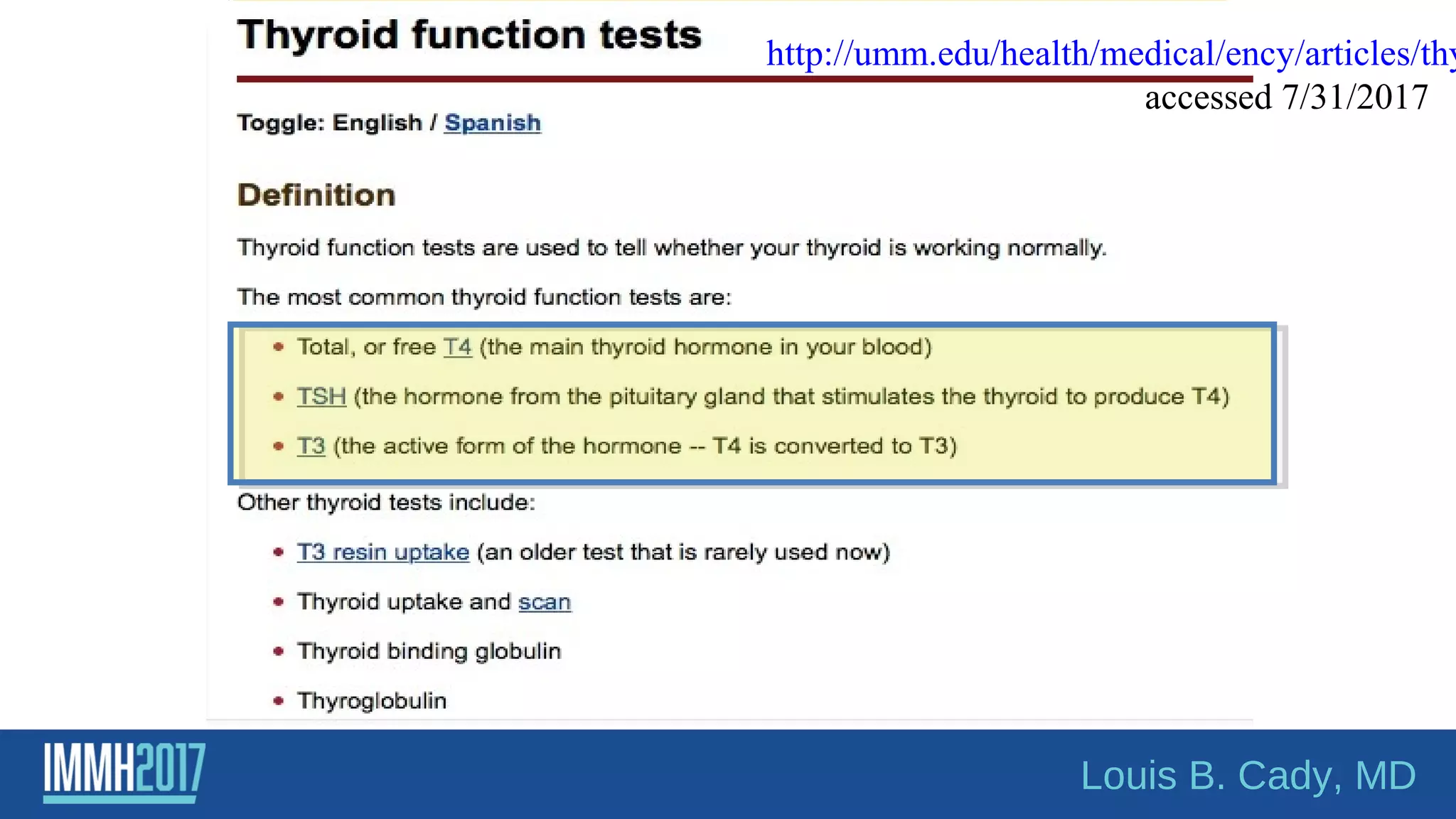
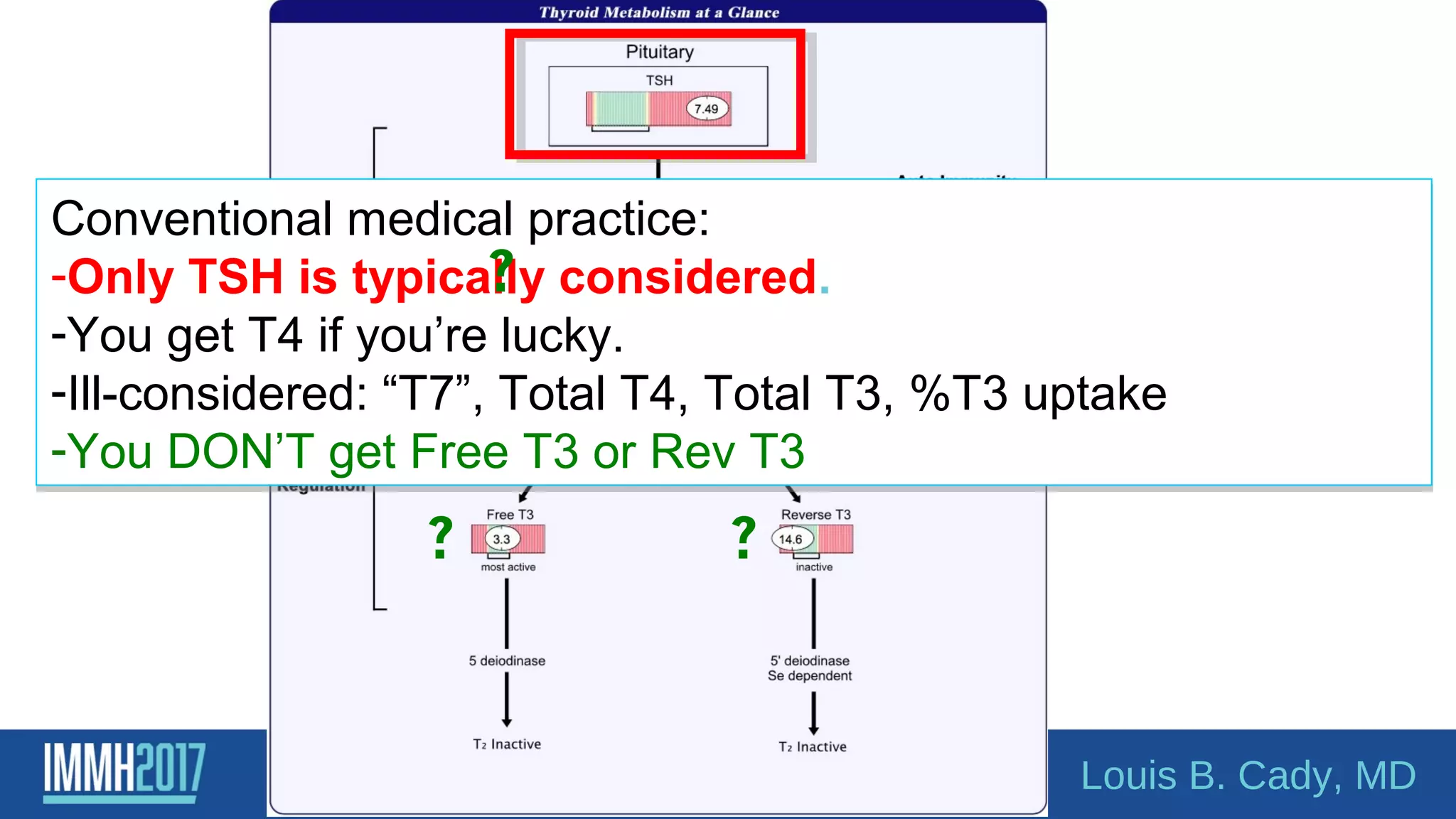
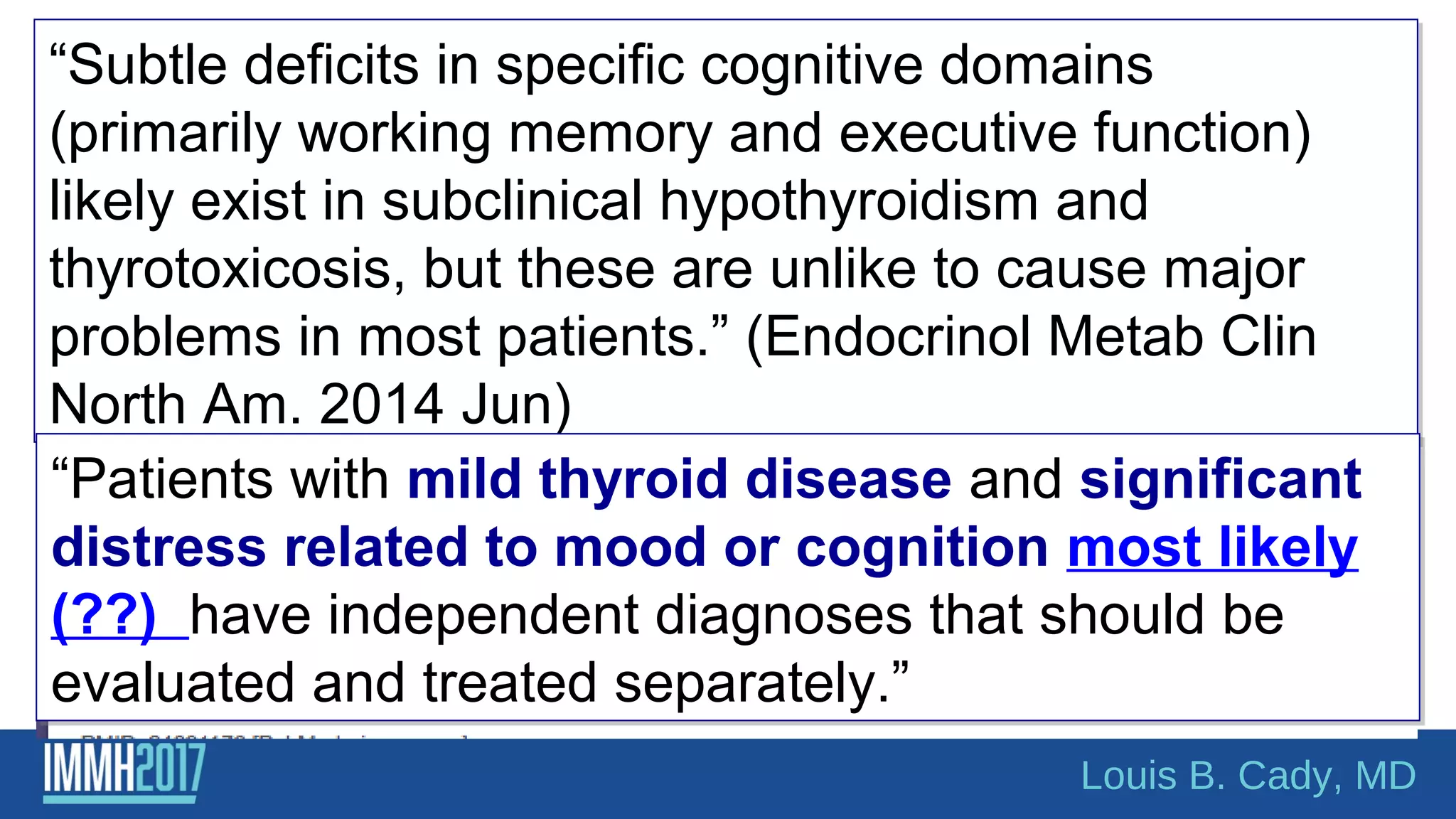
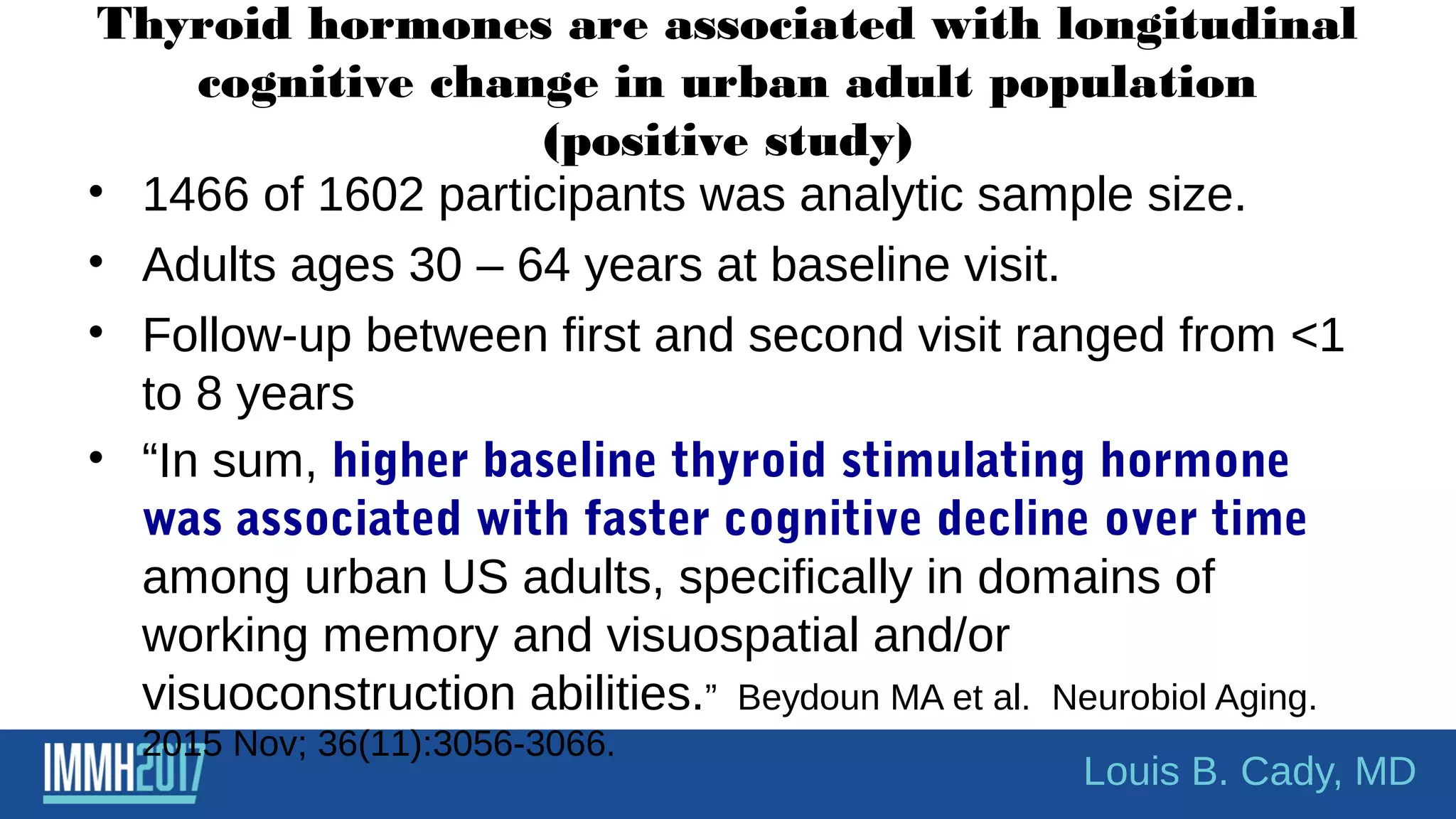
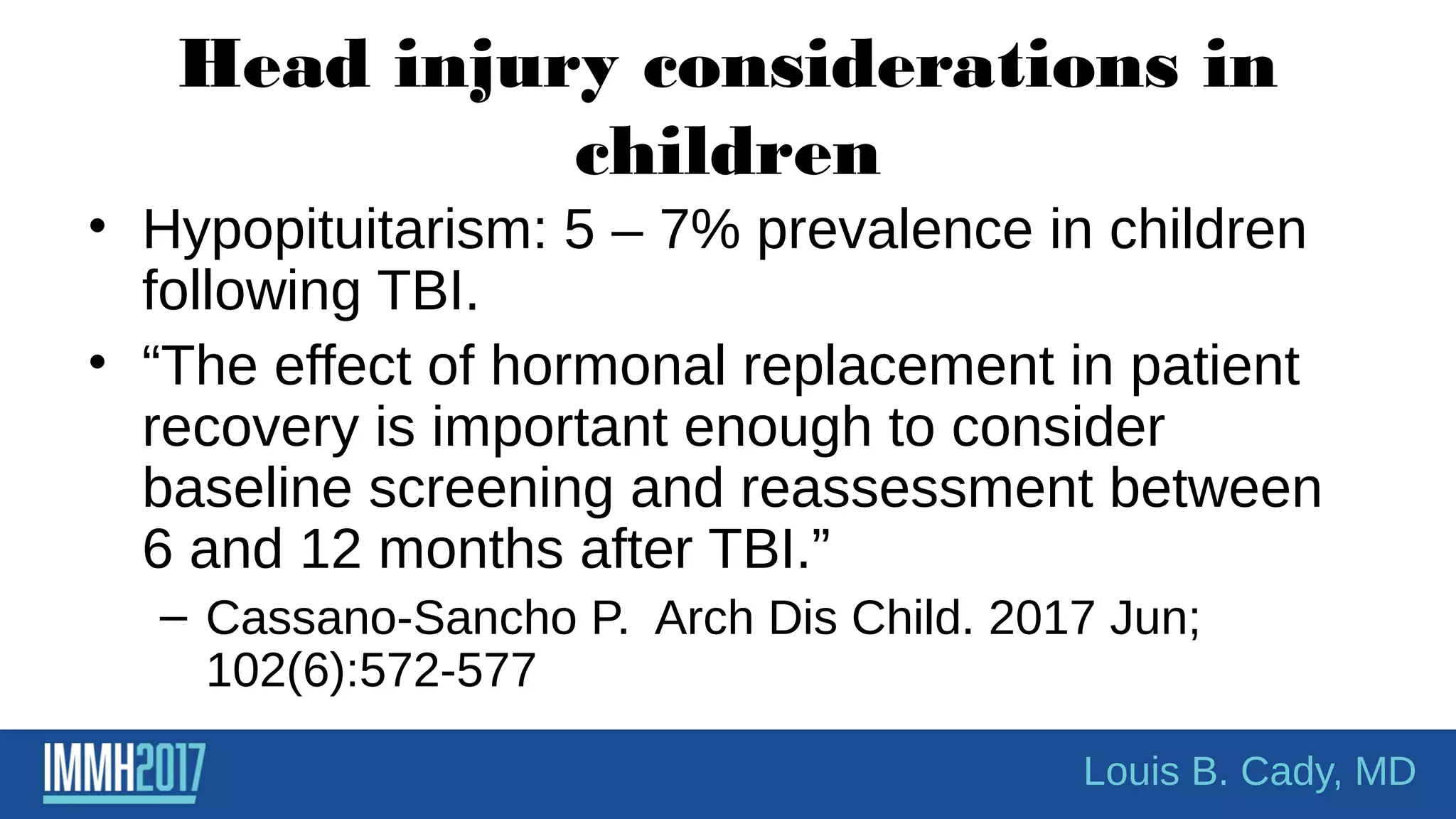
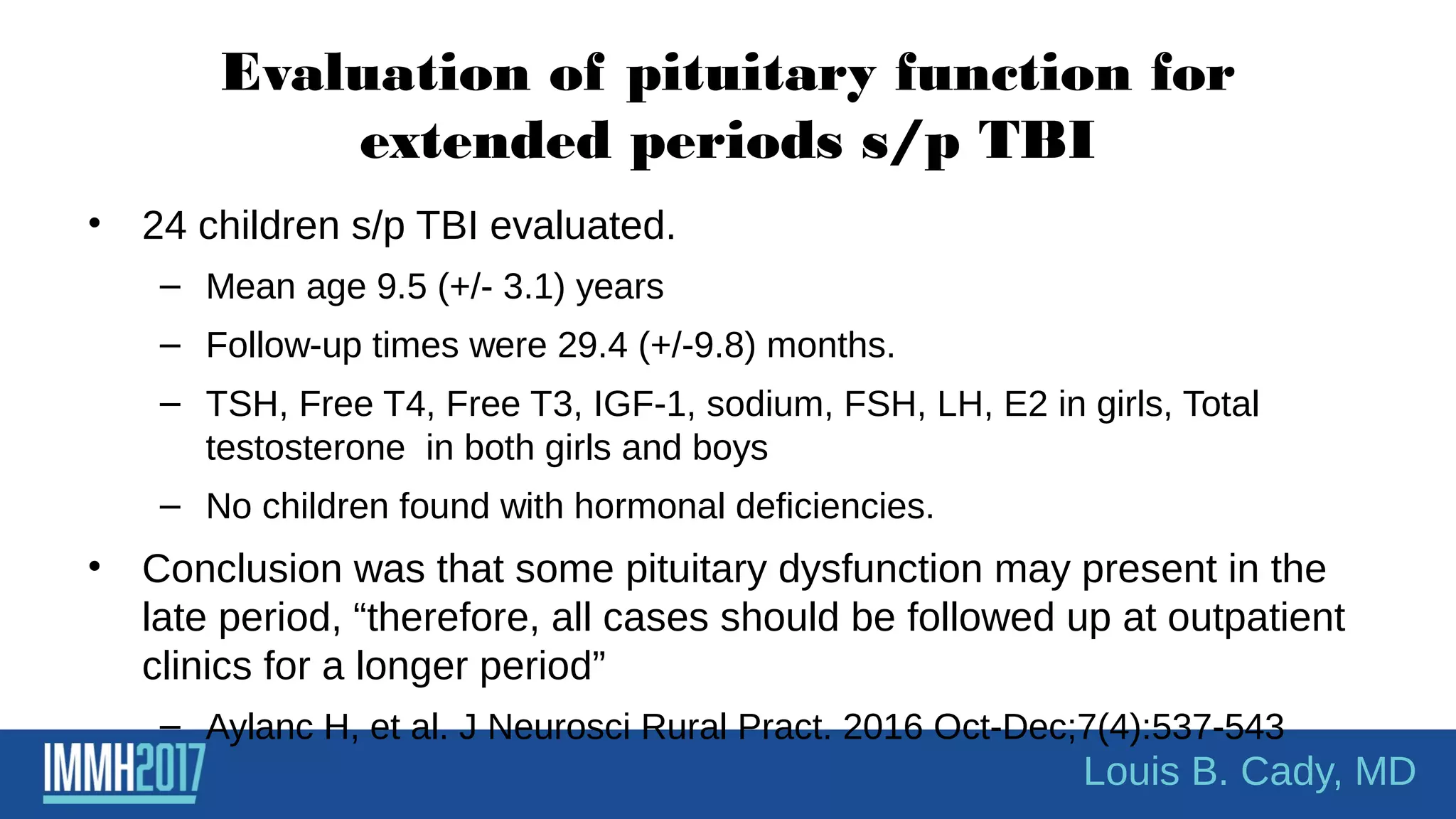
The document discusses the relationship between thyroid function and psychiatric conditions, particularly depression. It highlights various studies indicating that thyroid hormone augmentation can enhance the effectiveness of antidepressants and outlines the potential affects of thyroid dysfunction on mental health. Additionally, it critiques conventional medical practices regarding thyroid assessment and emphasizes the complexity of diagnosing and treating thyroid-related psychiatric disorders.
![CONCLUSIONS: This is the first study to
demonstrate associations between CBCL-DP
[Child Behavior Checklist Dysregulation Profile]
and subclinical hypothyroidism.
Louis B. Cady, MD](https://image.slidesharecdn.com/thyroidinmymindwithexpandedappendix-170928211840/75/Thyroid-IN-My-Mind-with-Expanded-Appendix-18-2048.jpg)
![Louis B. Cady, MD
“subclinical hypothyroidism bipolar disorder” 5/26/2017
42 citations
• “Thyroid abnormalities occur frequently in patients with BD regardless of
treatment.” [Lambert CG et al. Bipolar Disord. 2016 May;18(3):247-60]
• Patients with SCH had poorer performance than patients without SCH in
measures of verbal memory, attention, language, and executive functions.
[Martino DJ, et al. Subclinical hypothyroidism and neurocognitive
functioning in bipolar disorder. J Psychiatr Res. 2015 Feb;61:166-7]
• “There is no significant association between hypothyroidism and bipolar
disorder.” Menon B. Hypothyroidism and bipolar affective disorder: is
there a connection. Indian J. Psychol Med. 2014 Apr;36(2):125-8
• Hypothyroidism, either overt or more commonly subclinical, appears to the
commonest abnormality found in bipolar disorder. Chakrabarti S. Thyroid
functions and bipolar affective disorder. J Thyroid Res. 2011;2011;
2011:306367.](https://image.slidesharecdn.com/thyroidinmymindwithexpandedappendix-170928211840/75/Thyroid-IN-My-Mind-with-Expanded-Appendix-20-2048.jpg)

![[ http://www.umm.edu/patiented/articles/how_serious_hypothyroidism_000038_6.htm -
accessed August 2015 and 08 20 2016]
• “Thyrotropin (Thyroid-Stimulating Hormone or TSH).
Measuring TSH is the most sensitive indicator of
hypothyroidism.” (hunh?!) – accessed 9/5/2011
• “…blood tests for measuring levels of TSH
and free thyroxine (T4) are the only definitive
way to diagnose hypothyroidism” –
10/6/2012
Louis B. Cady, MD](https://image.slidesharecdn.com/thyroidinmymindwithexpandedappendix-170928211840/75/Thyroid-IN-My-Mind-with-Expanded-Appendix-24-2048.jpg)
![What does
Thyroid
receptor alpha1
bind?
Louis B. Cady, MD
Effectively:
-These genes make THR alpha
-THR Alpha is a nuclear receptor for
tri-iodothyronine [T3].
-“[This receptor] has been
shown to mediate the
biological activities of
thyroid hormone.”
Source: Gene ID: 7067, updated 9-Jul-2017](https://image.slidesharecdn.com/thyroidinmymindwithexpandedappendix-170928211840/75/Thyroid-IN-My-Mind-with-Expanded-Appendix-36-2048.jpg)

![Subclinical hypothyroidism in
the US– what’s the latest?As of August 6, 2015
• Synthesis: treat only those with TSH >10
– Hennessey JV Espaillat R. Diagnosis and management of Subclinical
Hypothyroidism in Elderly Adults: A Review of the Literature. J Am
Geriatr Soc. 2015 Jul 22. epub ahead of print
• Synthesis: SCH [TSH >/= 4.5- 19.99] associated with hip and other
fractures.
– Blum MR et al. Subclinical thyroid dysfunction and fracture risk: a meta-
analysis. JAMA. 2015 May 26;3(20):2055-65.
• Synthesis: Treatment of SCH [TSH 4-11] improved risk of
coronary heart dz risks. “Direct evidence on the benefits and
harms of screening remains unavailable.”
– Rugge JB et al. Screening for and treatment of thyroid dysfunction: An evidence
review for the US. Rockville (MD) Agency for Healthcare Research and Quality
(IS);2014 Oct. Report No. 15-05217-EF-1.](https://image.slidesharecdn.com/thyroidinmymindwithexpandedappendix-170928211840/75/Thyroid-IN-My-Mind-with-Expanded-Appendix-50-2048.jpg)
![As of August 21, 2016NEW LITERATURE – AUGUST 2016 – “Association between serum
thyrotopin levels and mortality among euthyroid adults in the United
States. [Inoue K et al. Thyroid. 2016 Aug 18 [Epub ahead of print]
•Population – NHANES III study . N = 12,584 adults>/= 20 years of age.
•Associations between TSH tertiles (high, medium, and low) and
mortalities (all cause, cardiovascular and cancer)
•Mean followup = 19.1 years with 3,395 deaths.
•Increase risk of all-cause mortality found in high normal TSH
compared to medium normal TSH group. ( Low normal compared to
medium also had higher all cause mortality).
•“This study indicated that the normal range of TSH levels may require
reevaluation.”
Louis B. Cady, MD](https://image.slidesharecdn.com/thyroidinmymindwithexpandedappendix-170928211840/75/Thyroid-IN-My-Mind-with-Expanded-Appendix-51-2048.jpg)
![Dr. Imre Zs-Nagy, MD – one more time!
Archives of Gerontology and Geriatrics, Volume 48, Issue 3, May-June 2009, 271-275
"[The] gerontological elite has instead sought to
obfuscate the facts ... the reason for this is
nothing less than an abject fear ... to avert their
loss of control, power, prestige, and position in
the multi-billion dollar industry of gerontological
medicine.”
Prof. Dr. Imre Zs.-Nagy, MD - part of the gerontology movement for four
decades; founder and Editor-in-Chief of the Archives of Gerontology and
Geriatrics](https://image.slidesharecdn.com/thyroidinmymindwithexpandedappendix-170928211840/75/Thyroid-IN-My-Mind-with-Expanded-Appendix-61-2048.jpg)
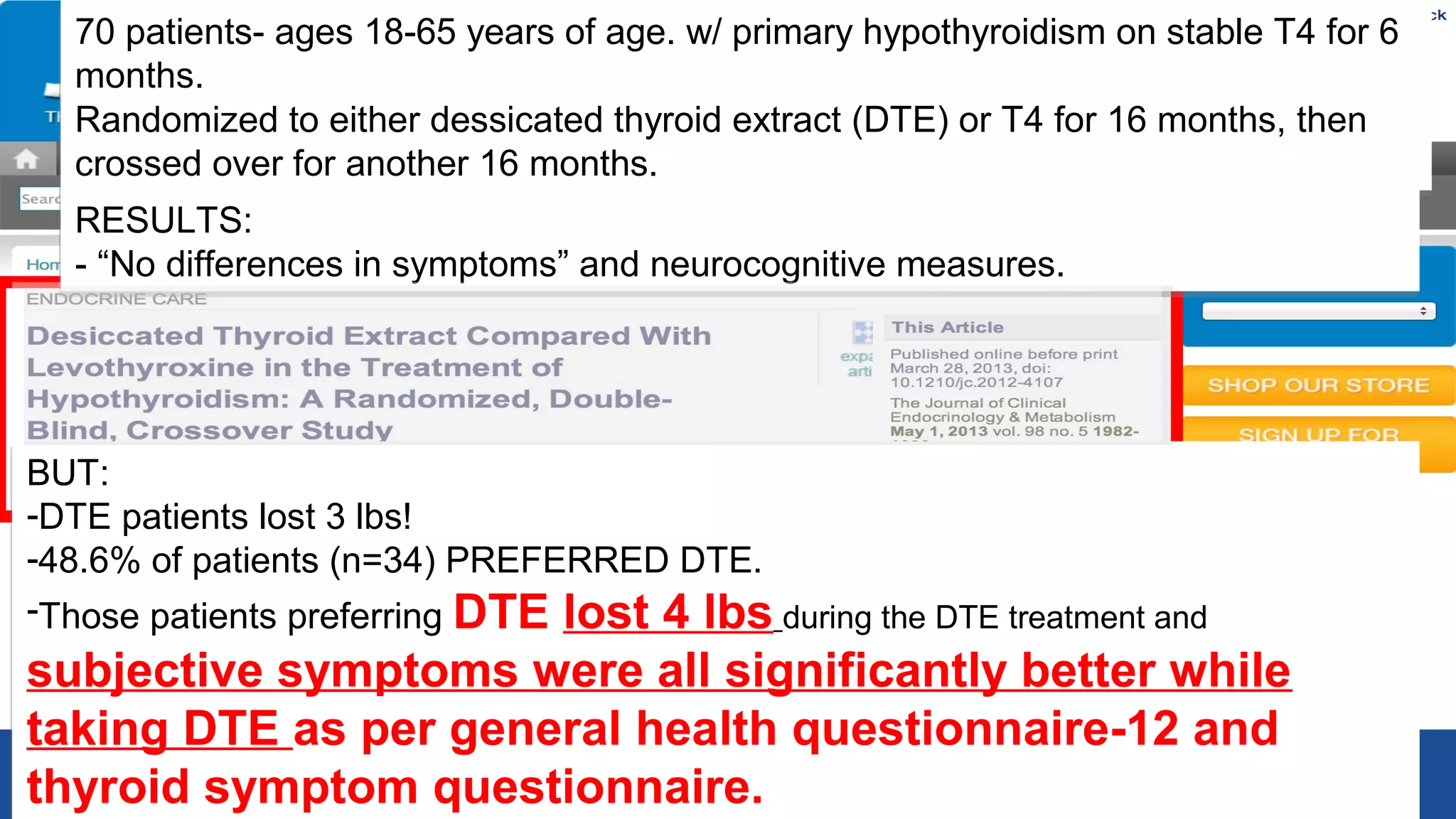
![“Conclusions”:
- DTE therapy did not result in a significant improvement in quality of life; however,
DTE caused modest weight loss and nearly half (46.8%) of the study patients
expressed preference for DTE over L-T4.
DTE therapy may be relevant for some hypothyroid
patients.” [Can you believe it????]
“Conclusions”:
- DTE therapy did not result in a significant improvement in quality of life; however,
DTE caused modest weight loss and nearly half (46.8%) of the study patients
expressed preference for DTE over L-T4.
DTE therapy may be relevant for some hypothyroid
patients.” [Can you believe it????]](https://image.slidesharecdn.com/thyroidinmymindwithexpandedappendix-170928211840/75/Thyroid-IN-My-Mind-with-Expanded-Appendix-66-2048.jpg)
![Framework:
• Decide where in the literature you want to be.
• Do you want to practice the way things “used to be” or do you
want to practice evidence based medicine?
– [or just blindly listen to the specialty societies who parrot from the
past?]
• Do you want your patient to be “normal” or “optimal”?
• And can you live with yourself and your decision?
Louis B. Cady, MD](https://image.slidesharecdn.com/thyroidinmymindwithexpandedappendix-170928211840/75/Thyroid-IN-My-Mind-with-Expanded-Appendix-70-2048.jpg)

![Other studies in children
• Endocrine-disrupting chemicals (EDC’s) and
perturb normal levels of hormones required for
normal neural circuit development.
– Three ubiquitous endocrine disruptors studied
[polychlorinated biphenyls, polybrominated diphenyl
esters, and bisphenol A.]
– Impact of these disrupts goes beyond relative
hypothyroidism and affect memory, cognition, and
social behavior.
– Pinson A et al. Andrology. 2016 Jul;4(4):706-22
Louis B. Cady, MD](https://image.slidesharecdn.com/thyroidinmymindwithexpandedappendix-170928211840/75/Thyroid-IN-My-Mind-with-Expanded-Appendix-89-2048.jpg)
![Prevalence of thyroid dysfunction and its
impact on cognition in older Mexican adults
(SADEM study)
• 1750 participants evaluated via interviews, TSH, and Free T4 levels.
– TSH of 0.4 – 4 was considered euthyroid.
– Over hypothyroidism = TSH>4.8
– Overt hyperthyroidism – TSH <0.3 IU/L
• Results:
– Overall estimated prevalence of thyroid dysfunction in Mexican
population was 23.7%.
• 15.4% we were classified as subclinical hypothyroidism.
– Thyroid dysfunction and cognitive impairment was most evident in
overt hypothyroidism [OR=1.261]
– Juarez-Decillo T et al. J. Endocrinol Invest. 2017 Mar 25.
Louis B. Cady, MD](https://image.slidesharecdn.com/thyroidinmymindwithexpandedappendix-170928211840/75/Thyroid-IN-My-Mind-with-Expanded-Appendix-94-2048.jpg)
![Somatotropic and thyroid hormones in the
acute phase of subarachnoid haemorrhage.
• Complicated hospital course was associated with
a deeper fall in TSH and T3 concentrations.
• “Low concentrations of TSH and T3 were
connected to worse SAH [subarachnoid
haemorrhage] grade and poor outcome.”
– Implications for treatment? No conclusions given.
– Zetterling M et al. Acta Neurochir (Wien). 2013
Nov;155(11):2053-62.
Louis B. Cady, MD](https://image.slidesharecdn.com/thyroidinmymindwithexpandedappendix-170928211840/75/Thyroid-IN-My-Mind-with-Expanded-Appendix-104-2048.jpg)
![Exogenous T3 administration provides
neuroprotection in a murine model of traumatic
brain injury.• Thyroid hormones noted to be decreased in patients with brain jury.
• Controlled cortical impact injury (CCI) [widely used experimentally]
was used in adult male mice.
• Tx with T3 (1/2 MICROgrams/100 grams body weight IP) one hour
after TBI resulted in a significant improvement in motor and
cognitive recovery after CCI.
• 24 hours after brain trauma, T3 treated mice showed significantly
lower number of apoptotic neurons.
• T3 significantly enhanced post-TBI expression of BDNF and GDNF
compared to control vehicle.
– Crupi R et al. Pharmacol Res. 2013 Apr;70(1):80-9.
Louis B. Cady, MD](https://image.slidesharecdn.com/thyroidinmymindwithexpandedappendix-170928211840/75/Thyroid-IN-My-Mind-with-Expanded-Appendix-105-2048.jpg)
![Multiple hormonal derangements seen as
determinant of cognitive decline in older men
• Thyroid, cortisol, and anobolic hormones [DHEA-
S, testosterone, and IGF-1] noted to decline with
age.
• Frailty related to consequences of cognitive
impairment and cognitive decline.
• Correlation with changes of thyroid hormone and
anabolic hormones in older men was found.
– Maggio M et al. J Nutr Health Aging. 2012
Jan;16(1):40-54.
Louis B. Cady, MD](https://image.slidesharecdn.com/thyroidinmymindwithexpandedappendix-170928211840/75/Thyroid-IN-My-Mind-with-Expanded-Appendix-106-2048.jpg)
![• “…levothyroxine replacement therapy with
vitamin E supplementation may ameliorate
cognitive deficit in PTU-induced
hypothyroidism [experimental model of
hypothyroidism] through the decrease of
oxidative stress status.”
• Note: BOTH were used.
– Pan T, et al. Endocrine. 2013 Apr;43(2):434-9.](https://image.slidesharecdn.com/thyroidinmymindwithexpandedappendix-170928211840/75/Thyroid-IN-My-Mind-with-Expanded-Appendix-110-2048.jpg)