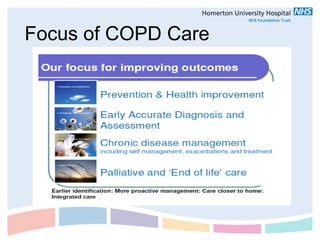
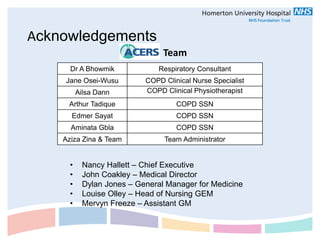
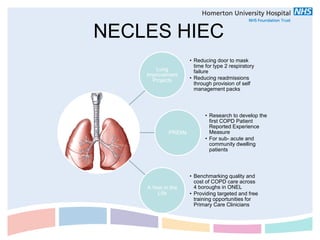
The document provides an overview of the ACERS (Acute COPD Early Response Service) team and COPD services in Hackney. The summary is:
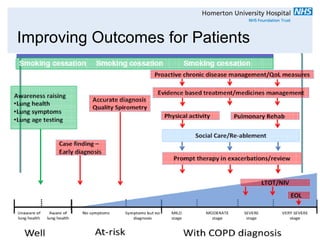
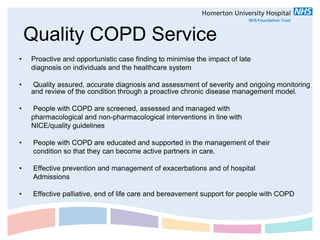
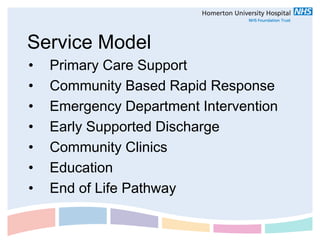
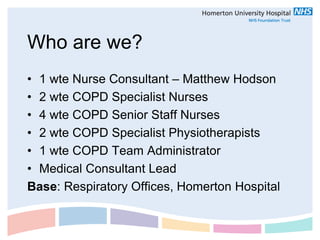
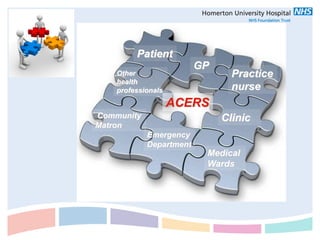
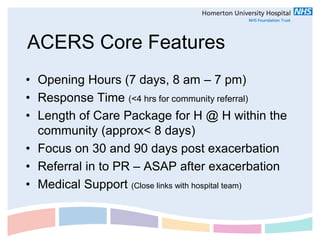
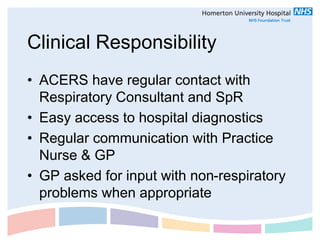
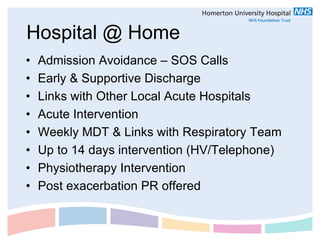
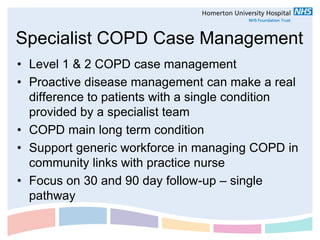
- The ACERS team introduces their service model which provides rapid community response for COPD exacerbations and ongoing chronic disease management.
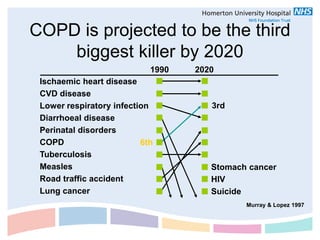
- COPD is projected to be the third leading cause of death by 2020. The ACERS team aims to provide comprehensive, integrated care to meet the needs of COPD patients in Hackney.
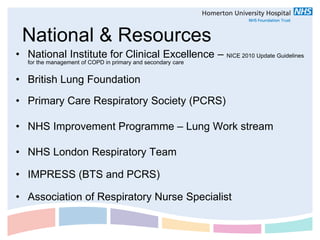
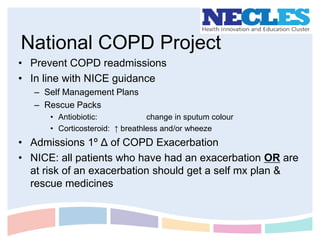
- Resources and support available include the NHS London Respiratory Team, British Lung Foundation, NICE guidelines, and the National COPD Project which focuses on reducing readmissions.


![Multidisciplinary working
– COPD care should be delivered by a multidisciplinary team that
includes respiratory nurse specialists & Specialist Ward Nurses
– Consider referral to specialist departments (not just respiratory
physicians)
Specialist department Who might benefit?
Physiotherapy People with excessive sputum
Dietetic advice People with BMI that is high, low or
changing over time
Occupational therapy People needing help with daily living
activities
Social services People disabled by COPD
Multidisciplinary palliative People with end-stage COPD (and their
care teams families and carers)
[2004]](https://image.slidesharecdn.com/copdpresentation-120207130851-phpapp02/85/COPD-presentation-21-320.jpg)