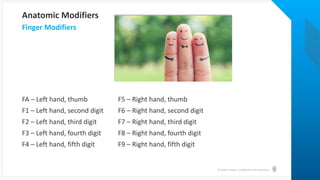
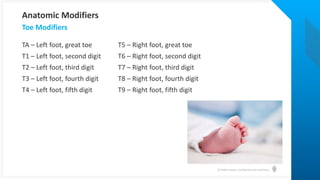
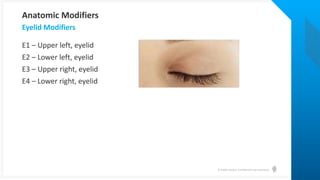
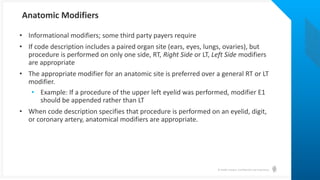
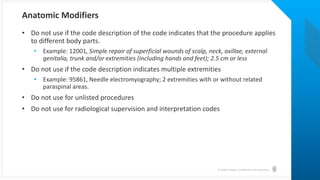
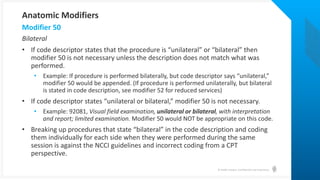
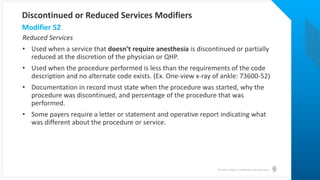
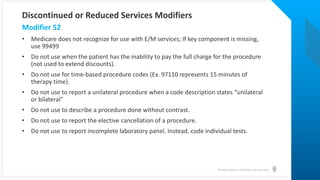
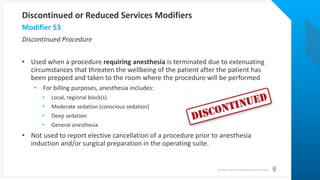
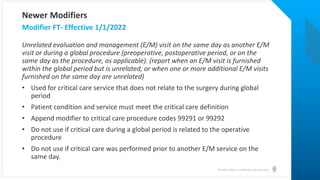
This guide provides essential information on the correct application of coding modifiers for medical services, emphasizing that modifier rules vary by payer and may impact reimbursement. It covers a variety of modifiers including evaluation and management (e/m) modifiers, anatomical modifiers, and those indicating discontinued or reduced services. The document includes specific examples and guidelines for properly coding to ensure accurate payment and compliance with regulations.

![© Health Catalyst. Confidential and Proprietary.
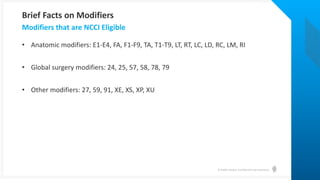
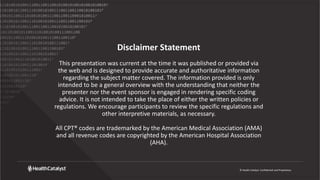
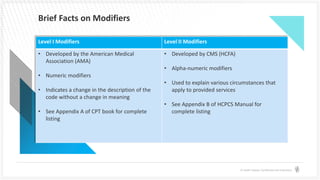
Brief Facts on Modifiers
• Rules for assigning modifiers vary from payer
to payer and between the different Medicare
Administrative Contractors (MACs)
• Modifier usage does not guarantee payment
• Certain modifiers can be used to override National Correct Coding Initiative (NCCI)
edits [aka Procedure to Procedure (PTP) edits]
• Use of certain modifiers will impact reimbursement. Use of “informational”
modifiers will provide information that will ease claim processing to avoid delays.](https://image.slidesharecdn.com/aphysician-focusedguidetoapplyingmodifierscorrectly-final-230313193016-39fb227e/85/Webinar-A-Physician-Focused-Guide-to-Applying-Modifiers-Correctly-5-320.jpg)