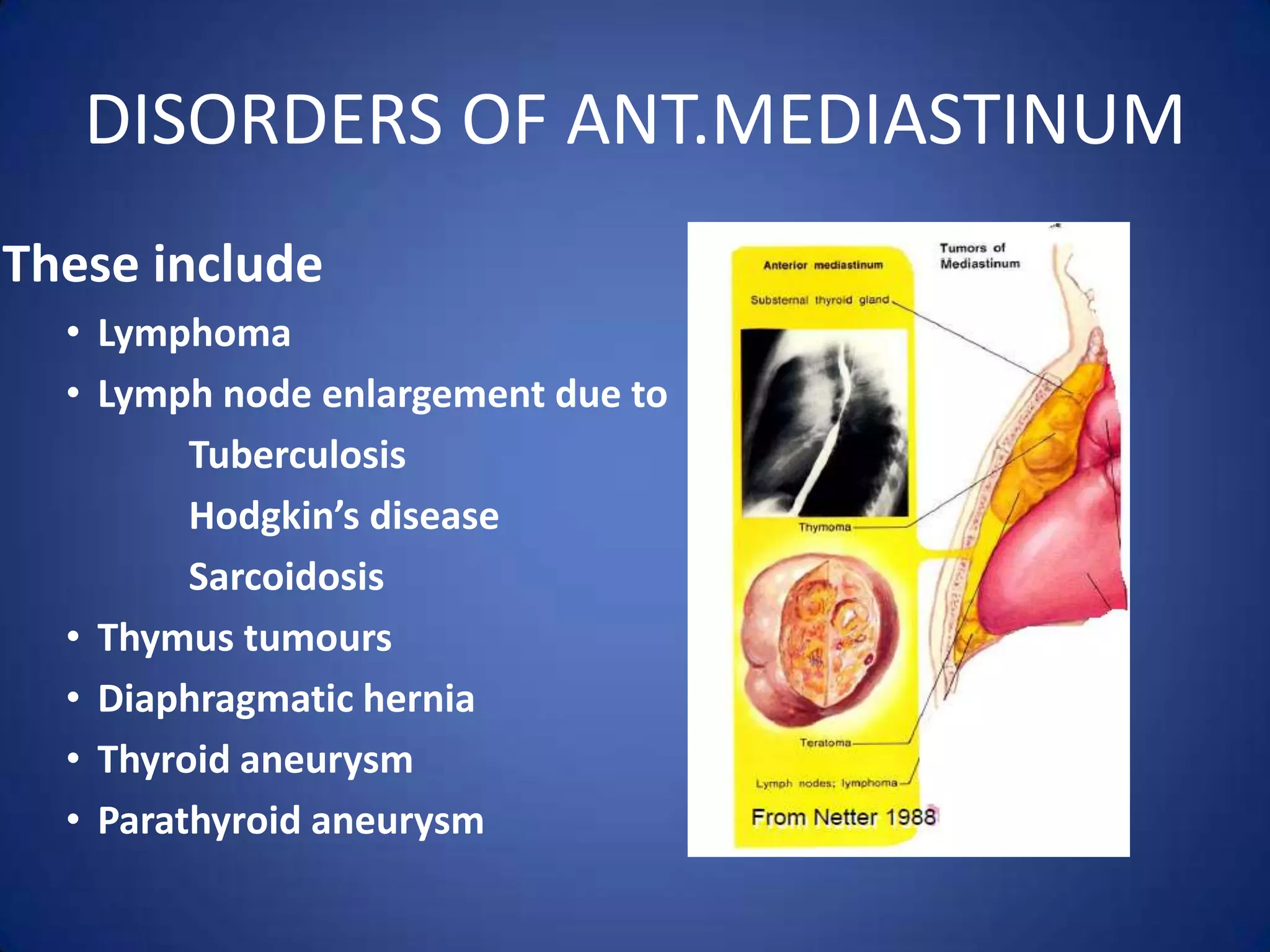
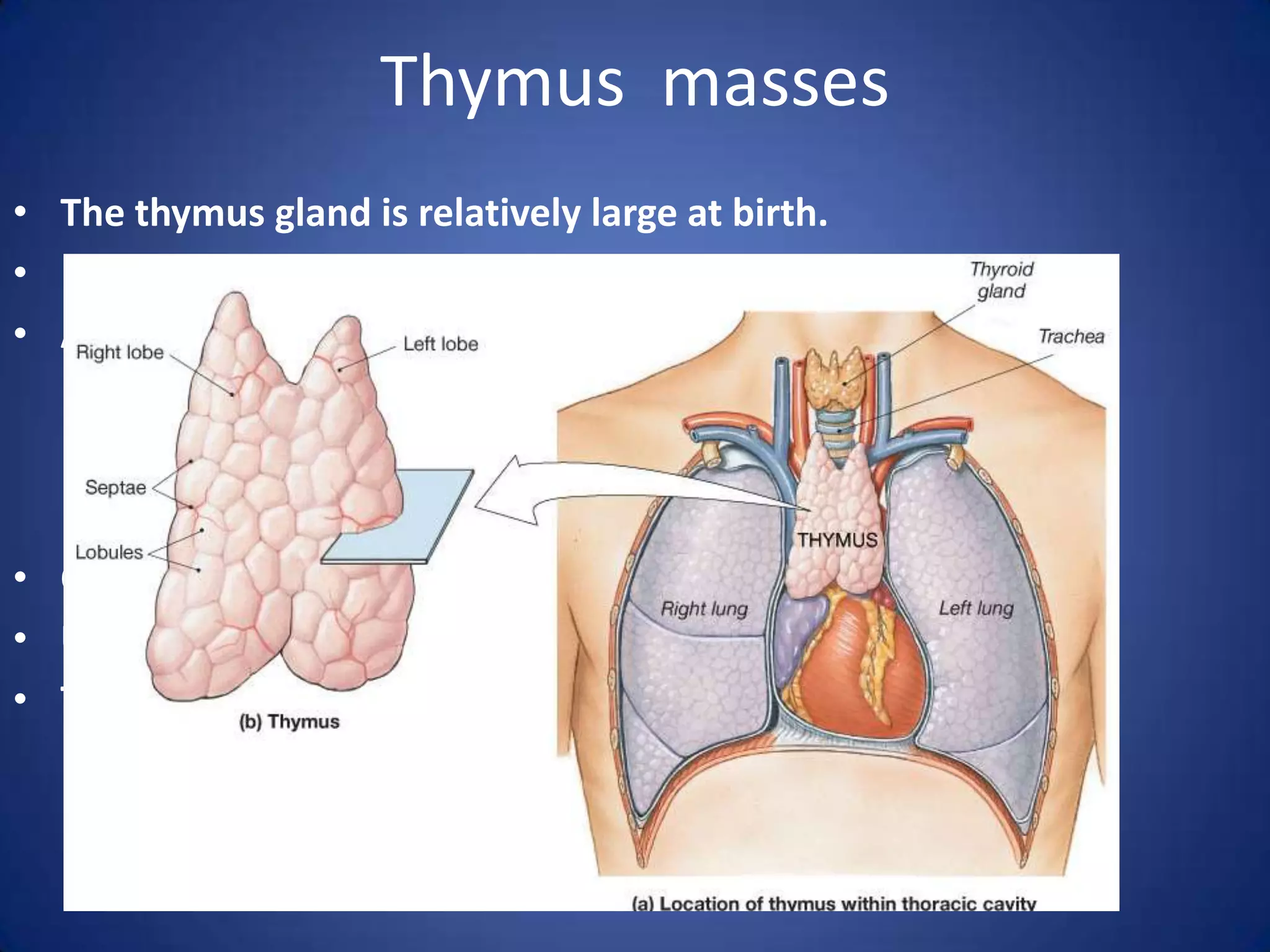
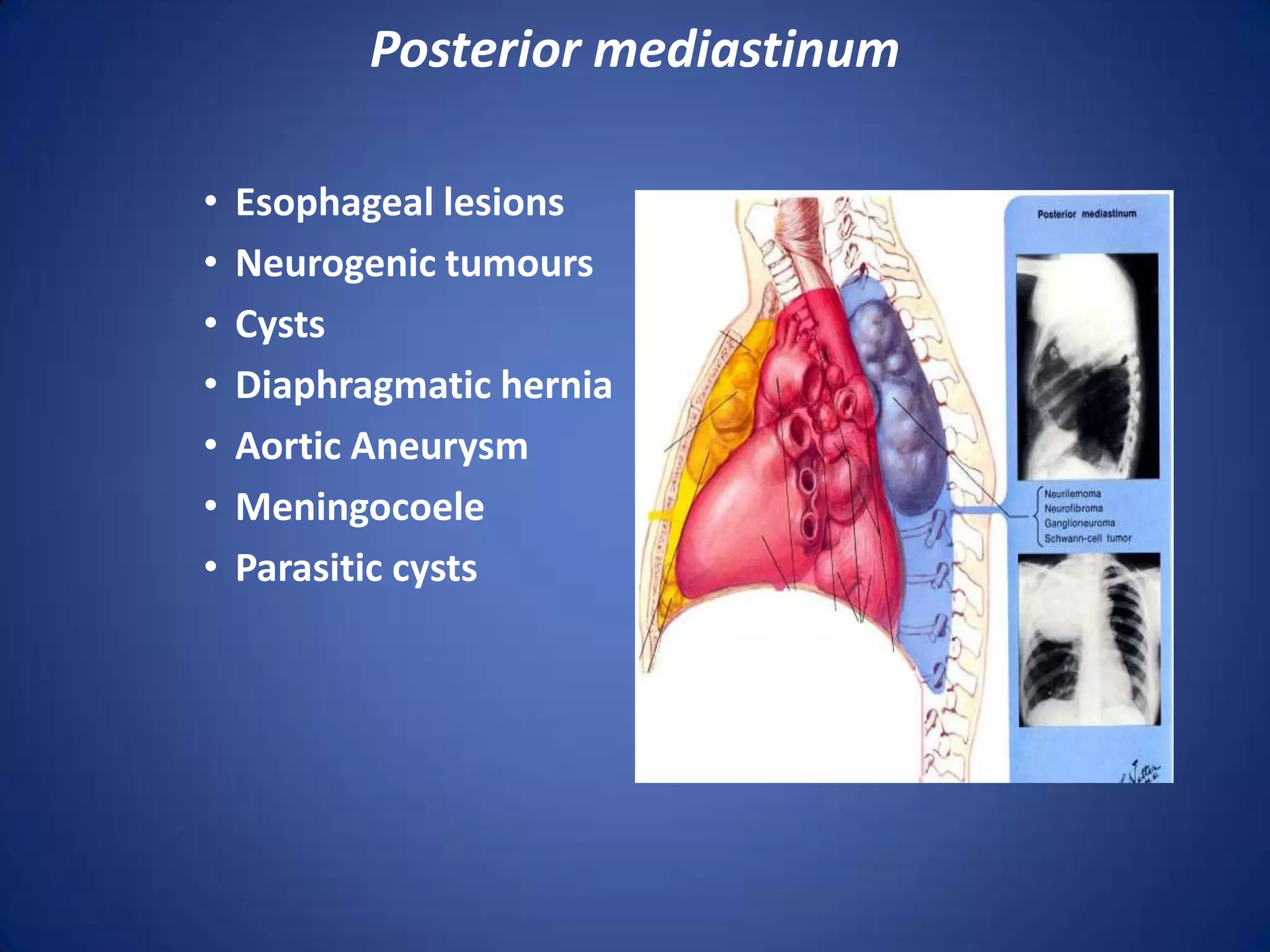
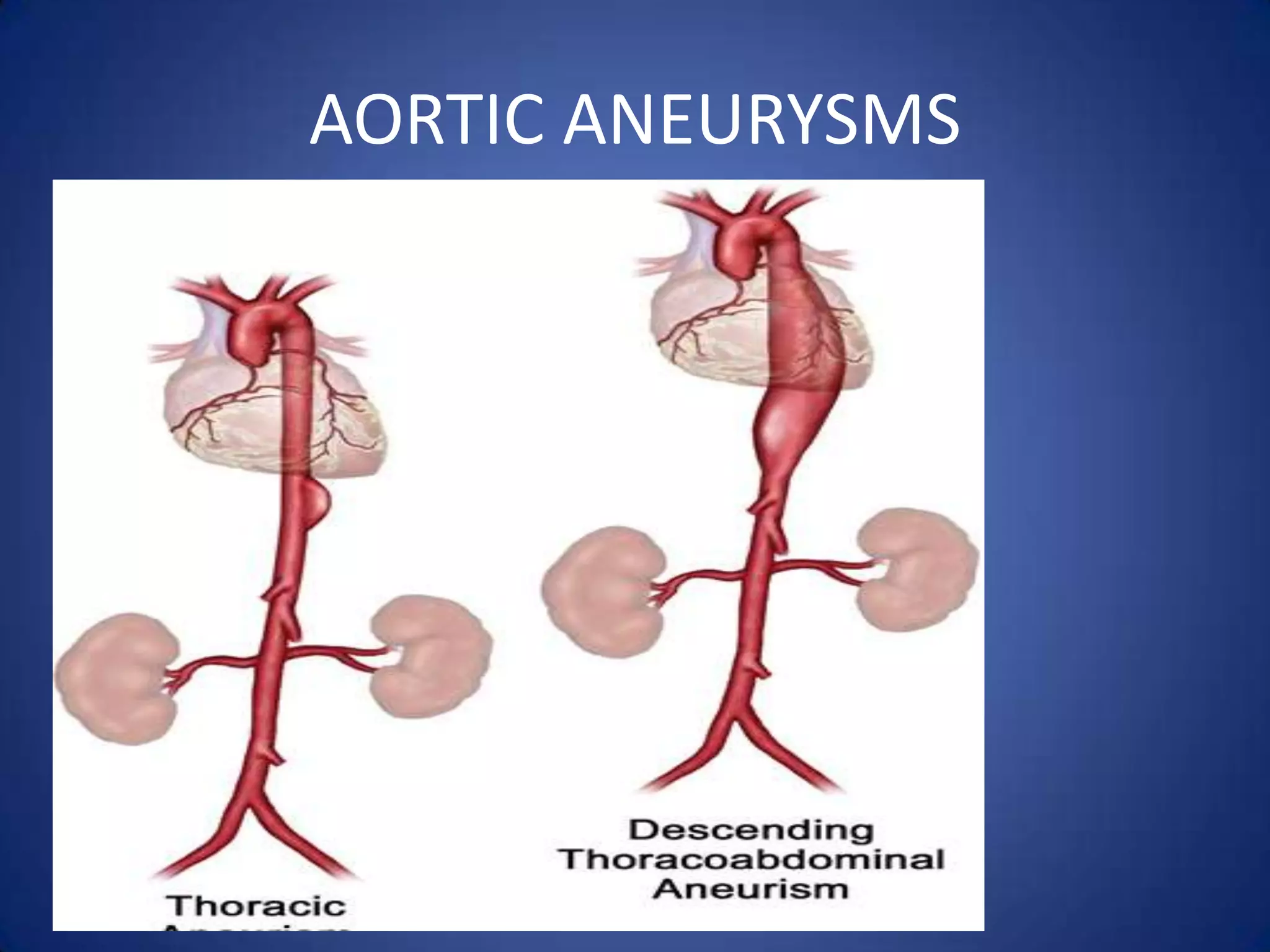
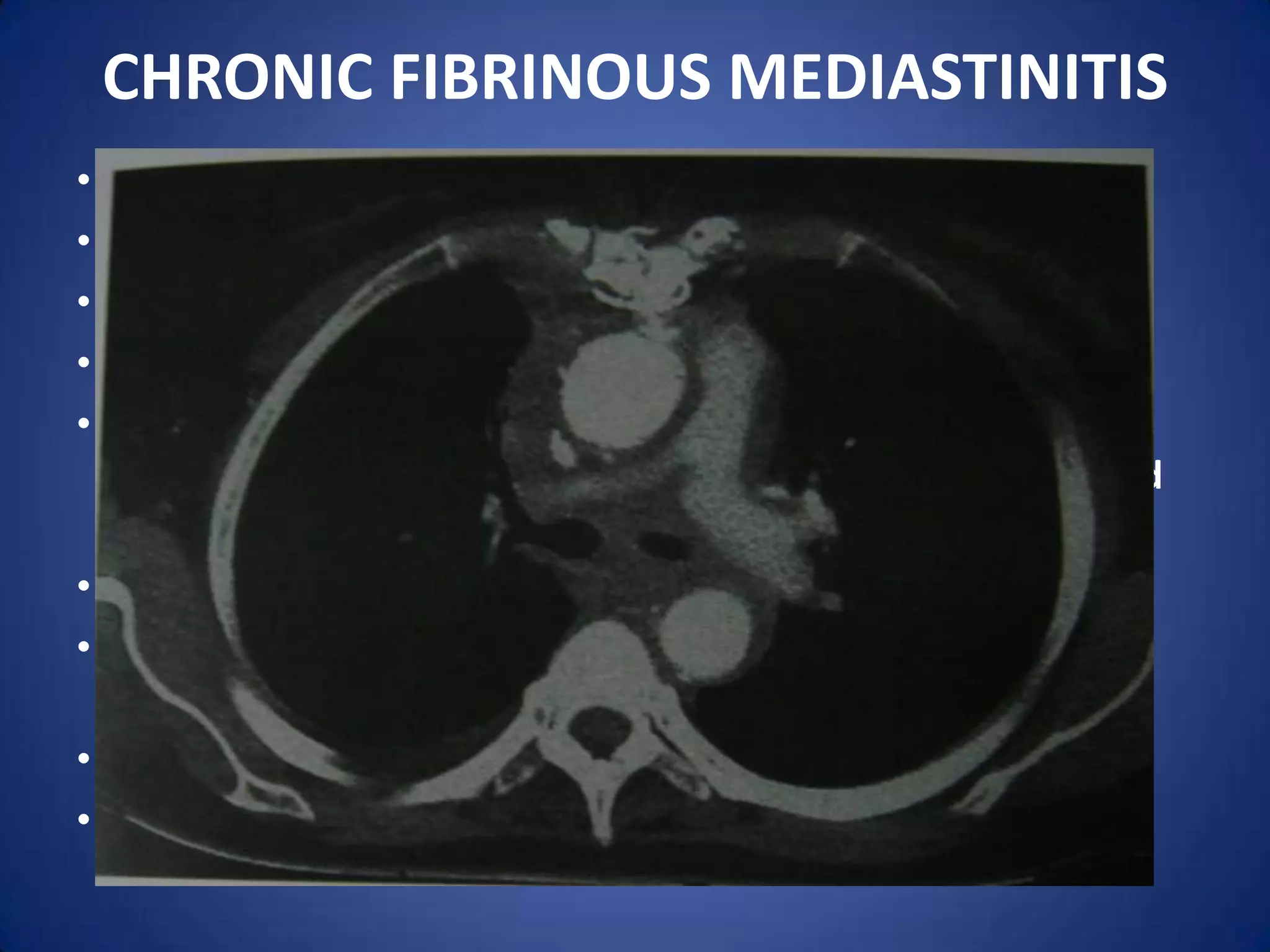
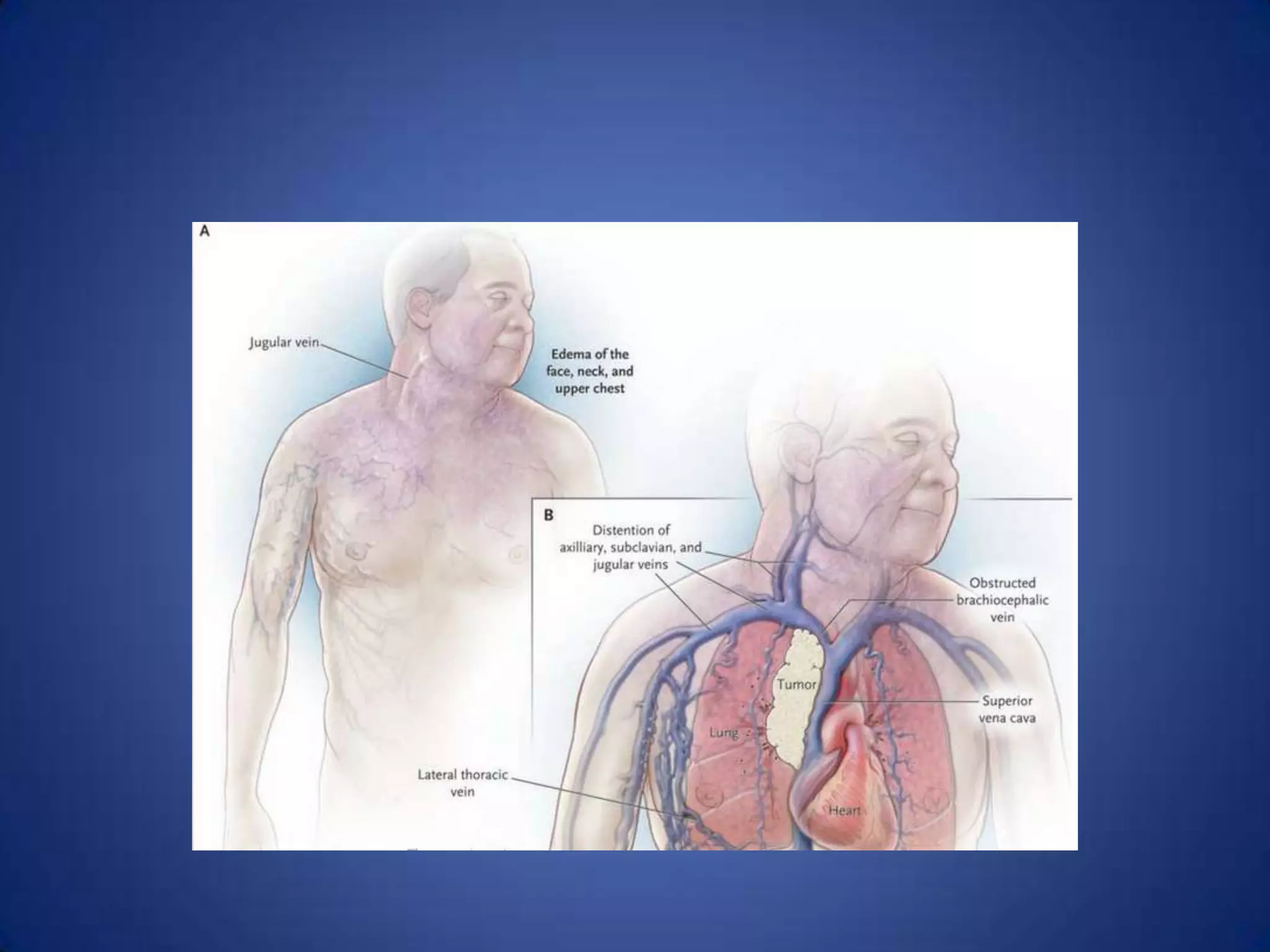
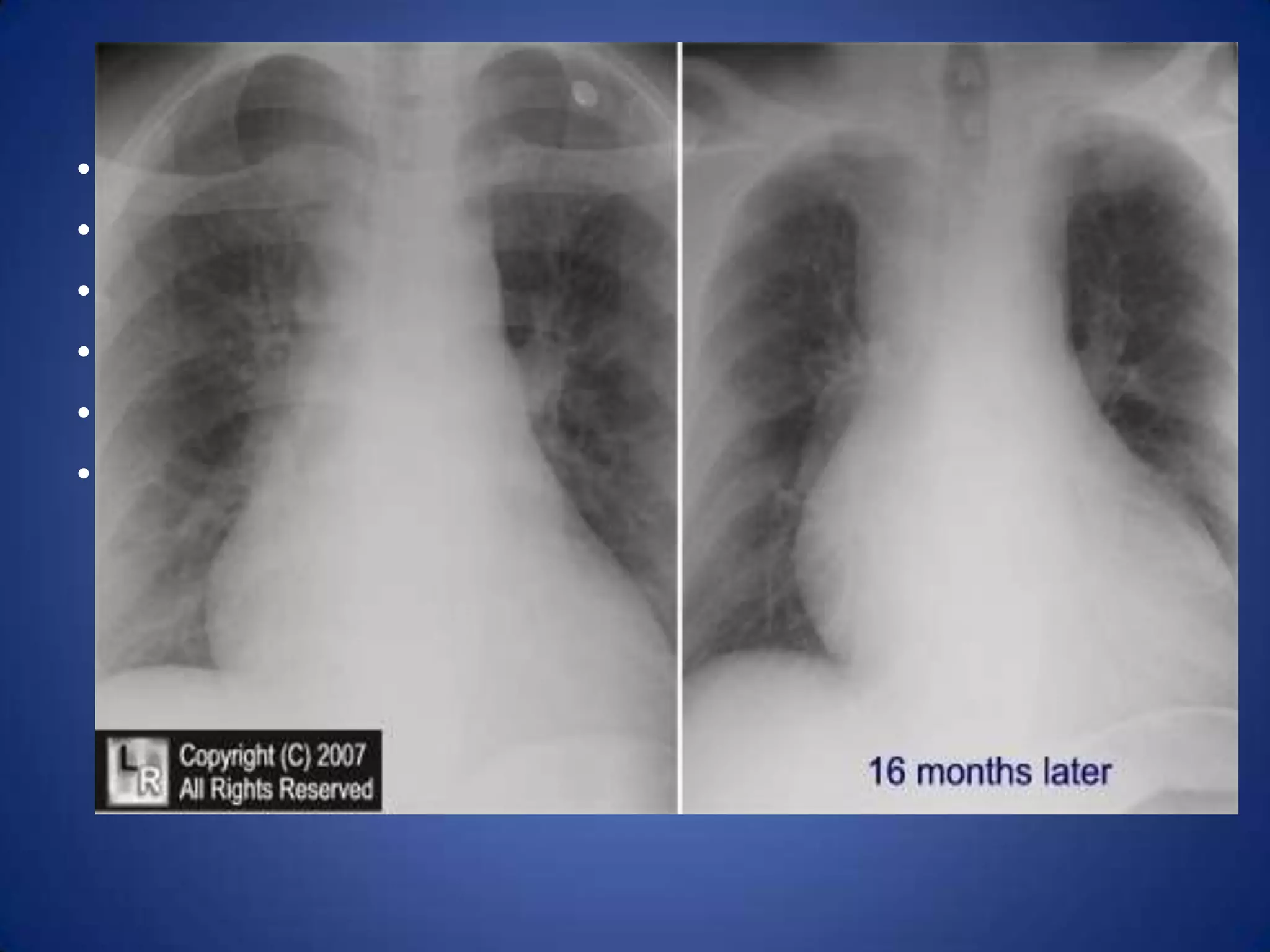
The document discusses the anatomy and disorders of the mediastinum. It begins by describing the anatomy of the different compartments of the mediastinum and structures contained within each. It then discusses various disorders that can arise in each compartment, including tumors, cysts, infections and others. Common tumors mentioned are thymoma, teratomas, and lymphomas. Clinical features, investigations, treatment and prognosis of different disorders are provided.