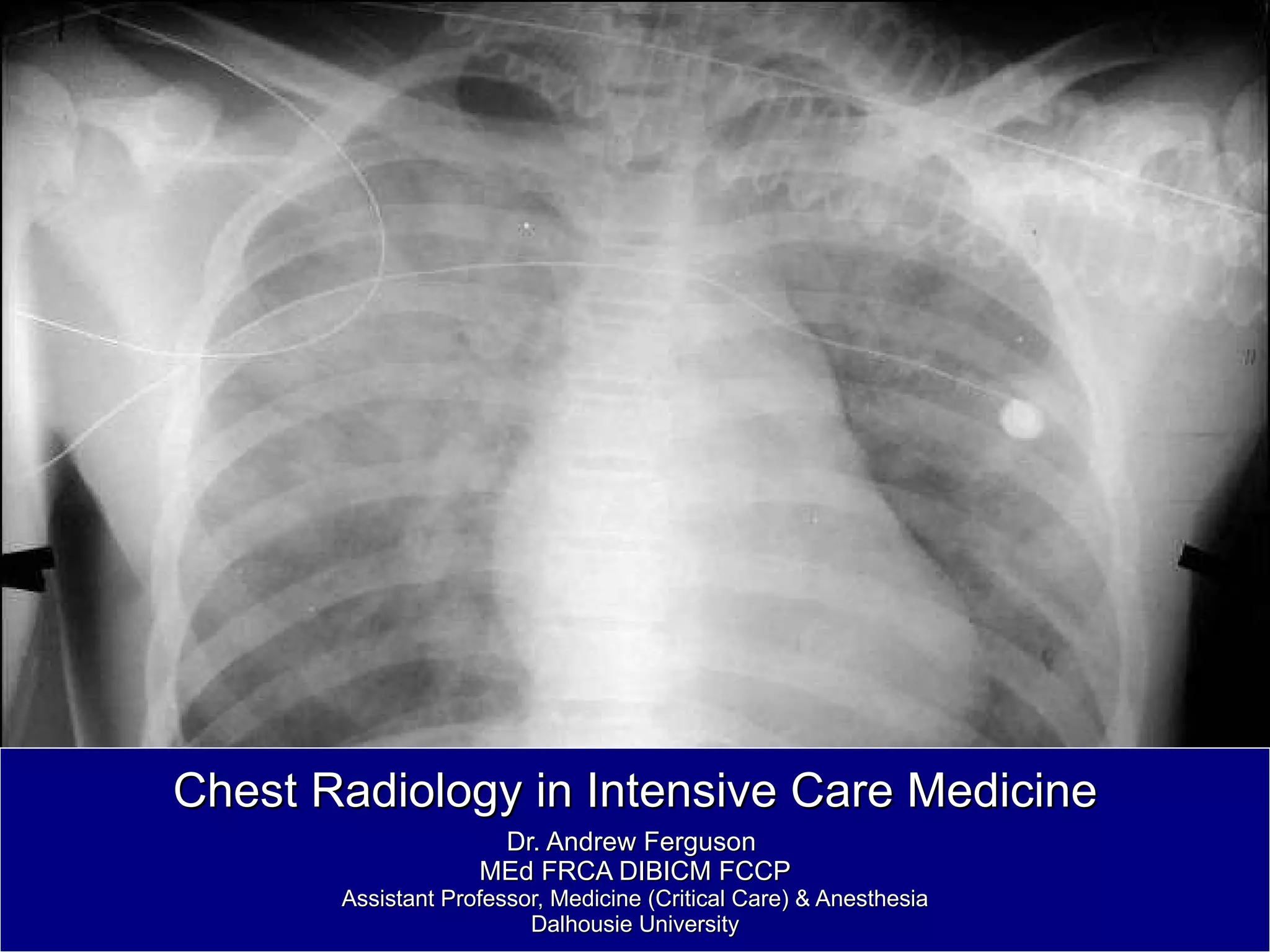
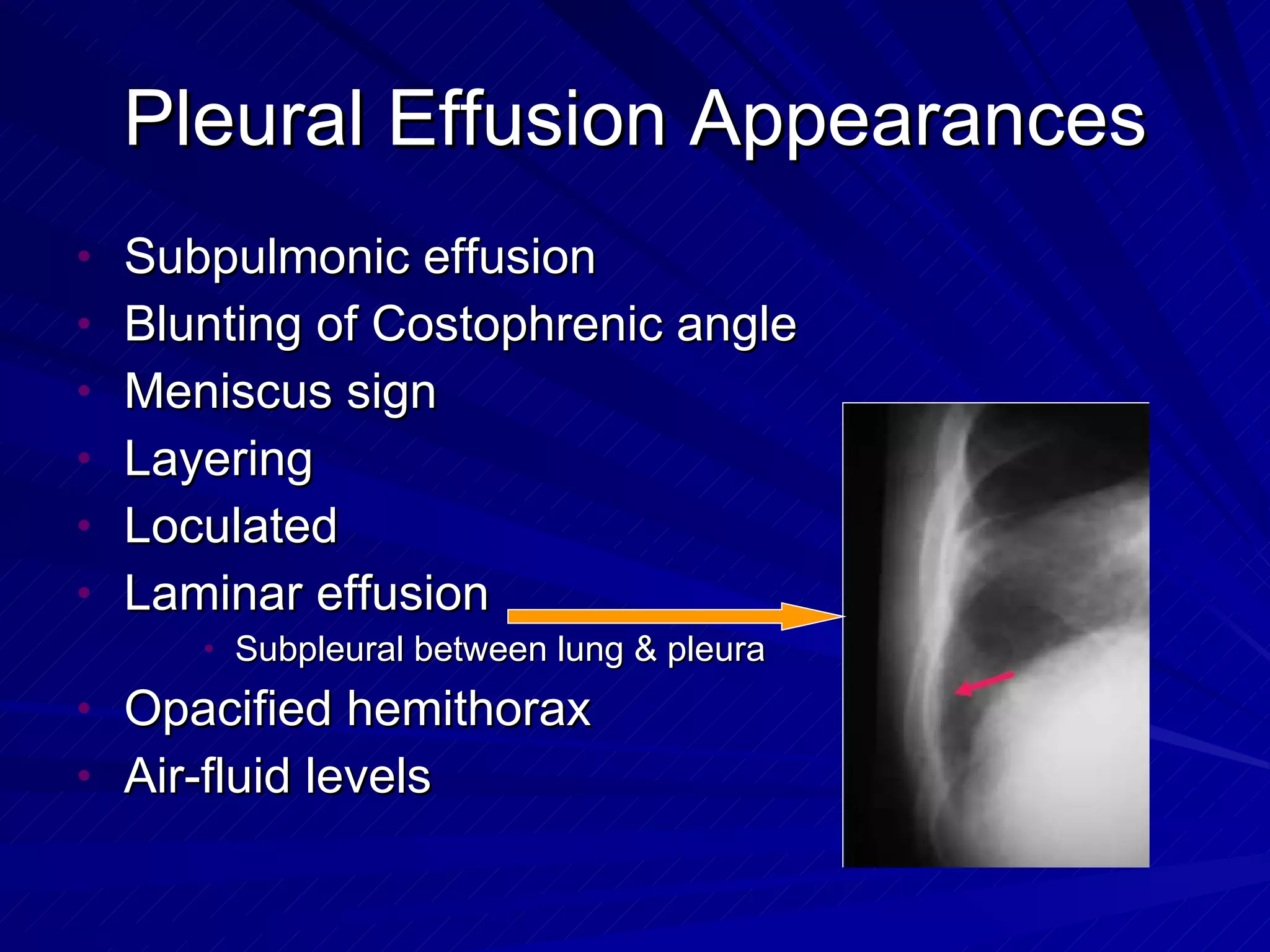
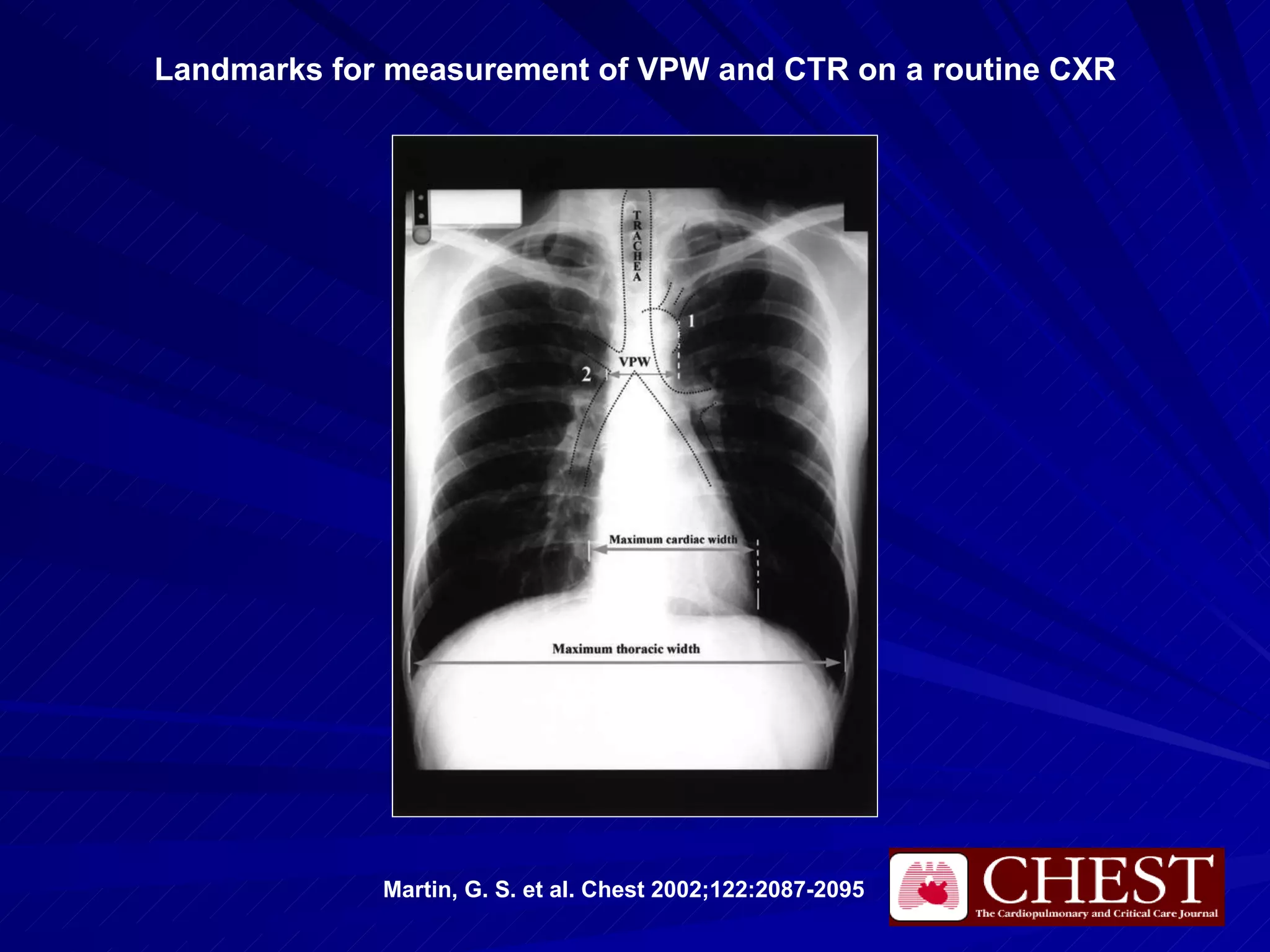
- Chest radiography is useful for assessing pulmonary edema, infiltrates, effusions, pneumothorax, and positioning of lines and tubes in intensive care patients. Common findings include air bronchograms, hilar enlargement, Kerley lines, and increased vascular pedicle width.
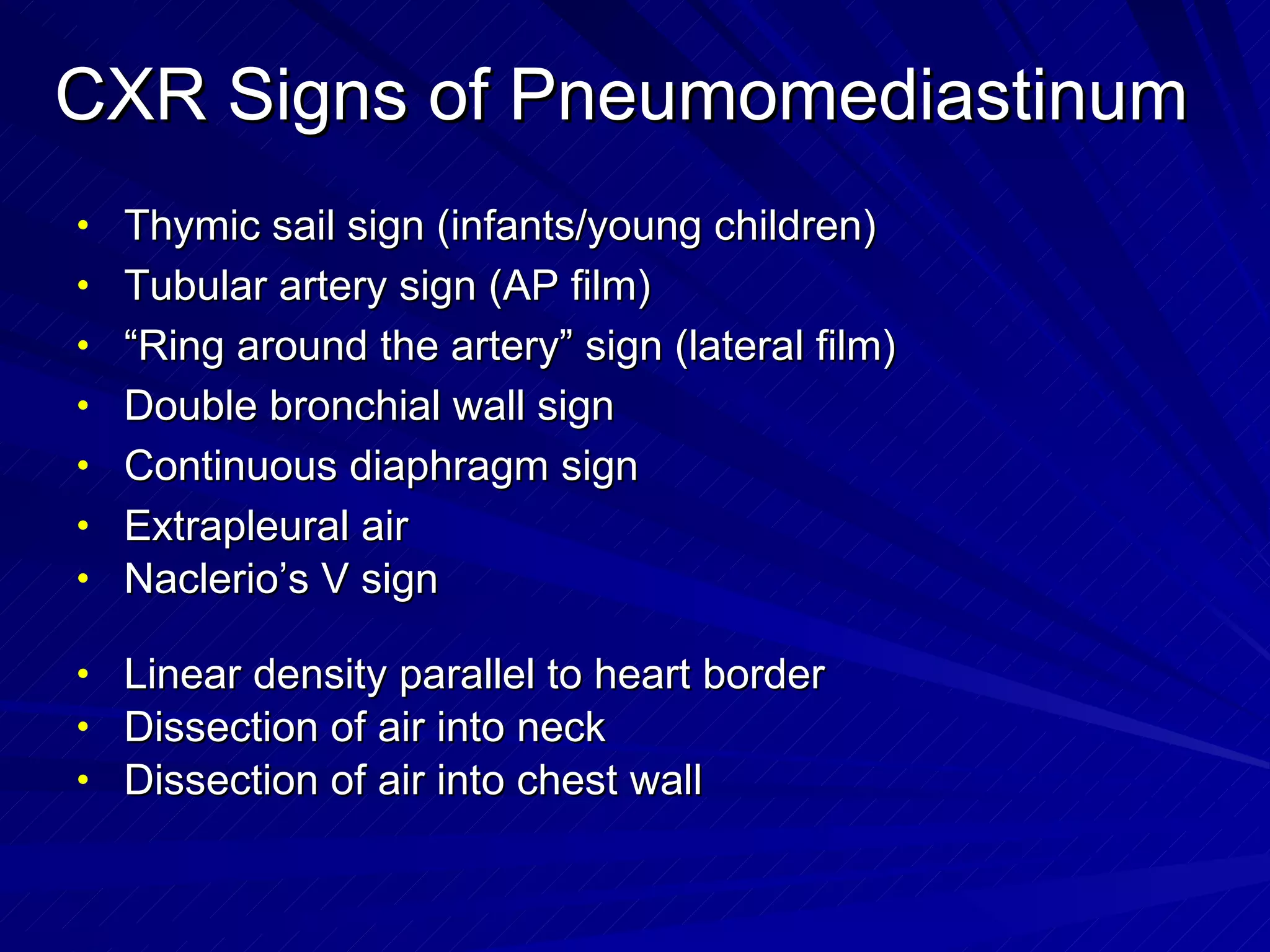
- Pneumomediastinum is suggested by findings like the continuous diaphragm sign, Naclerio's V sign, and double bronchial wall sign. A pneumothorax may be occult or demonstrated by a pleural line with absent lung markings.
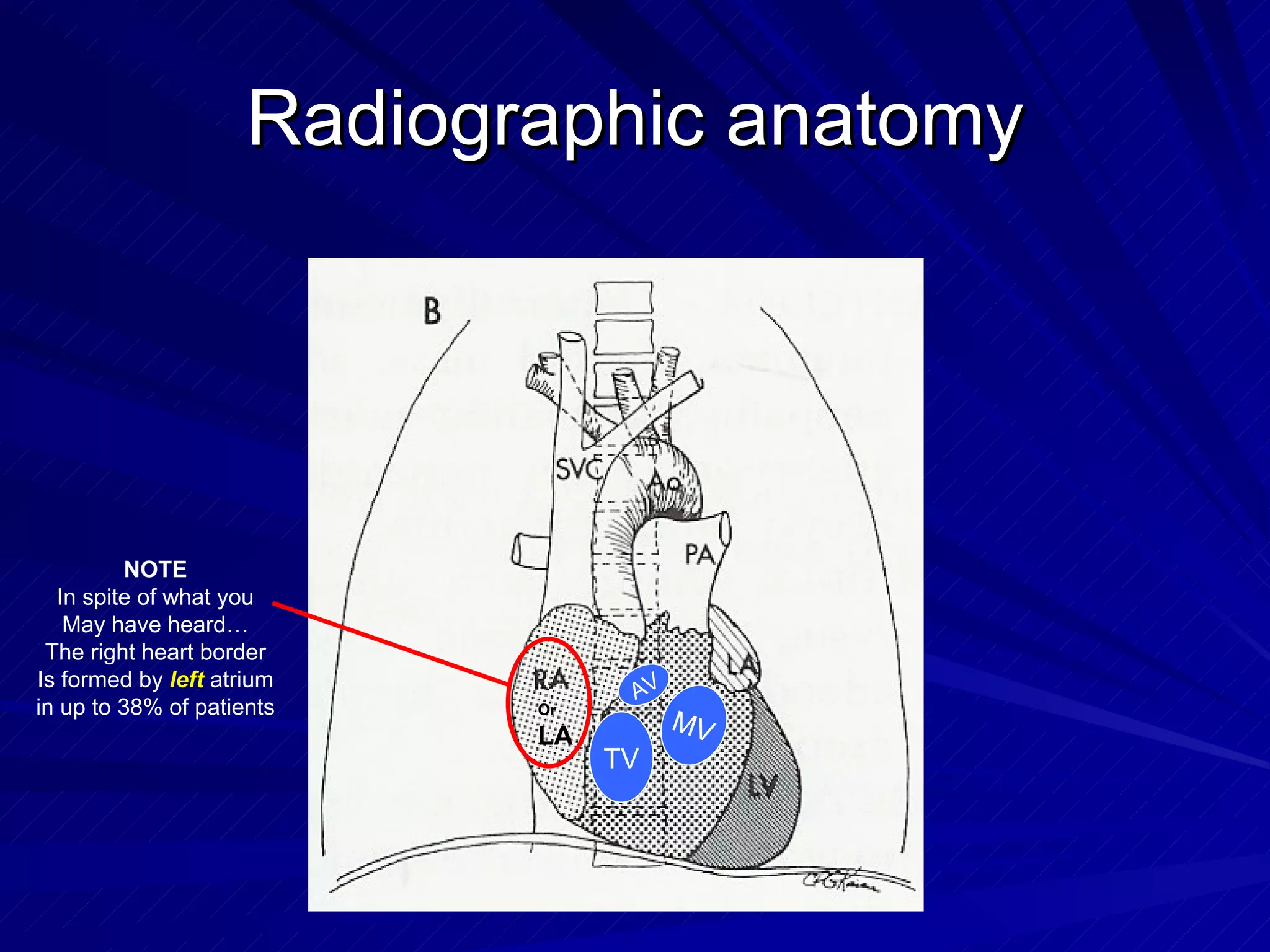
- Proper positioning of central lines is important but can be challenging due to anatomical variability. The tip should lie in the SVC above the pericardial