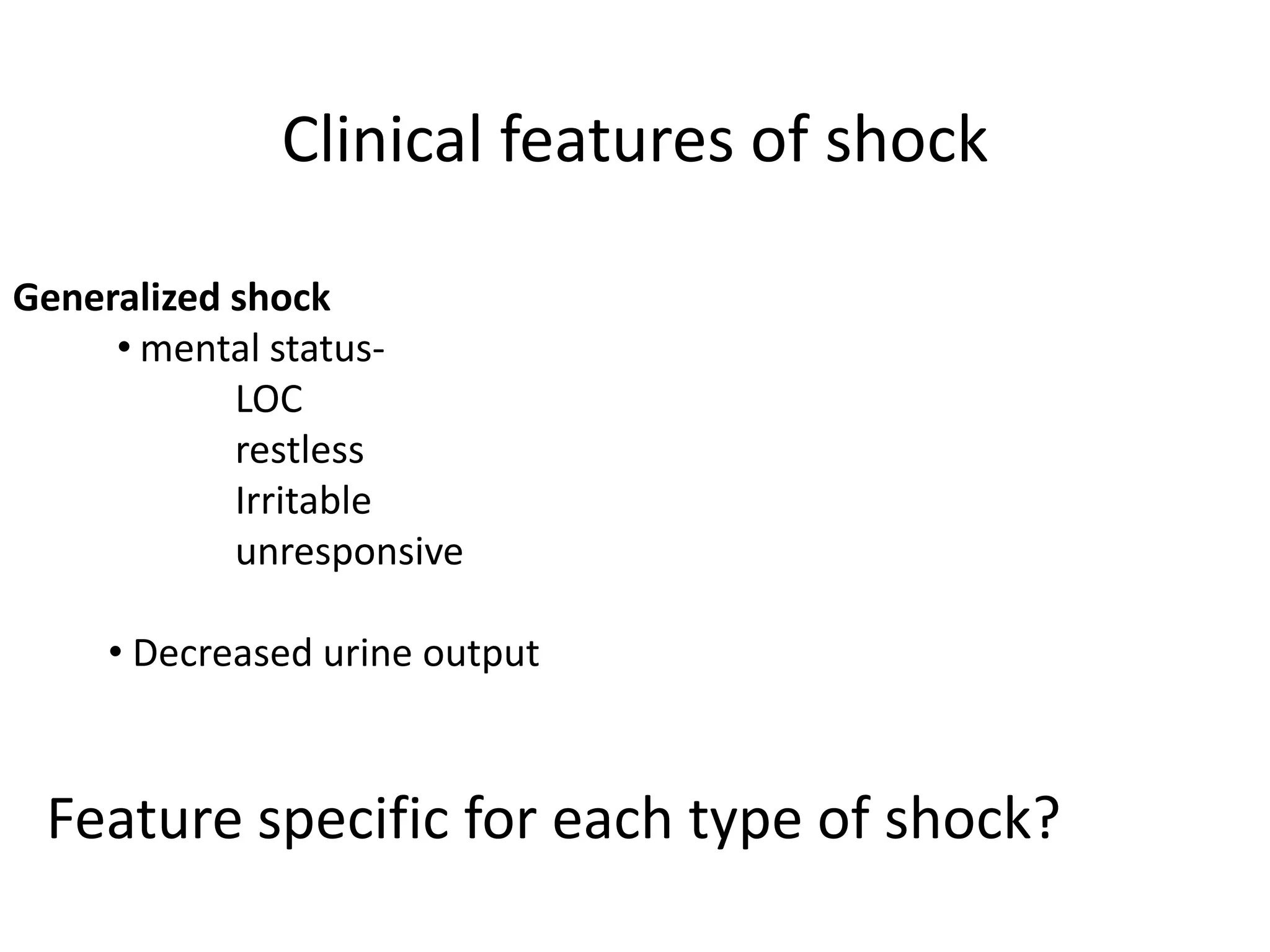
The document provides a comprehensive overview of different types of shock, including their pathophysiology, clinical features, and management strategies. It categorizes shock into several types: hypovolemic, cardiogenic, obstructive, septic, anaphylactic, and neurogenic, detailing their causes, symptoms, and appropriate treatments. Emphasis is placed on early recognition, fluid resuscitation, and specific interventions for each type of shock to restore tissue perfusion and prevent mortality.














![S/S vary depending on severity of fluid loss:
• 15%[750ml]- compensatory mechanism maintains CO
• 15-30% [750-1500ml- Hypoxemia, hypotension, generalized
vasoconstriction and reduction in urine output to 20-30
ml/hour.
• 30-40% [1500-2000ml] -Impaired compensation & profound
shock along with severe acidosis
hypotension, tachycardia over 120, tachypnoea, urine output
under 20 ml/hour and the patient is confused.
• 40-50% - refractory stage:
marked hypotension, tachycardia and tachypnoea. No urine
output and the patient is comatose
loss of volume= death](https://image.slidesharecdn.com/shock-160406142527/75/Shock-17-2048.jpg)







































