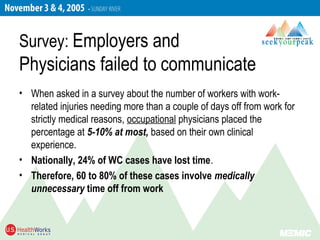
- Many lost workdays from injuries are preventable, but 60-80% involve non-medical factors prolonging time off. Effective communication between physicians, employers, and employees is key to addressing issues like motivational problems or poor workplace relationships that inhibit recovery.
- Physicians play an important role in injury management by diagnosing accurately, providing treatment plans, and accepting responsibility for addressing both medical and non-medical barriers to returning to work. Addressing just the medical factors is not enough.
- Preventing prolonged disability requires a cooperative approach where physicians obtain information from employers about job duties and employers help injured workers feel supported in returning to restricted work.





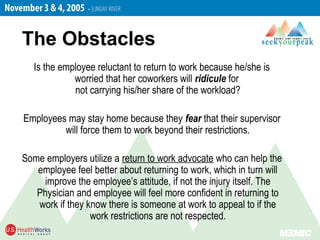
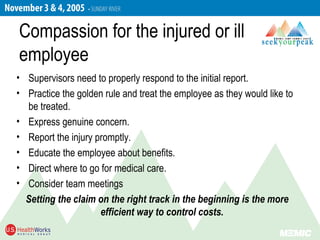
![Employer as a return to work advocate
• Someone to help recovering employees when their
supervisors are not meeting their needs.
• A staff person in health and safety, risk management,
or human resources. A company nurse, or the
company’s Physician. A previously injured “Model
Patient” employee.
• If not available, the role may end up being played by
the union or the injured employee’s lawyer. [Gulp!]](https://image.slidesharecdn.com/memiccompsummit2005template-171115122757/85/MEMIC-comp-summit-2005-33-320.jpg)