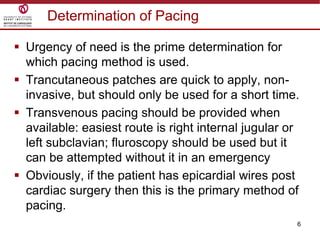
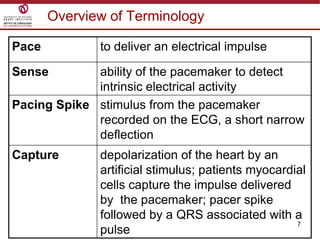
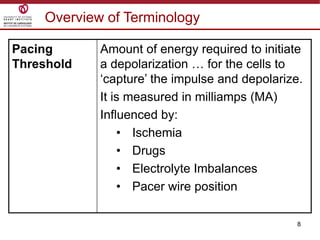
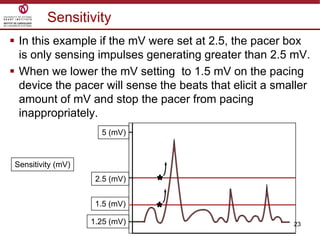
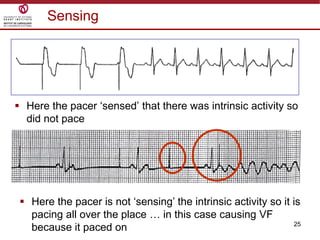
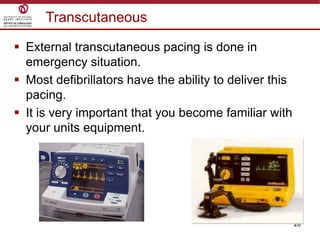
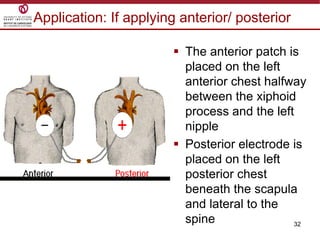
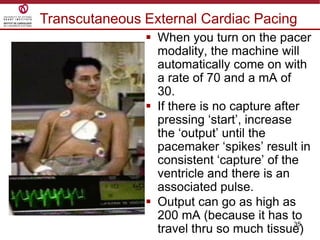
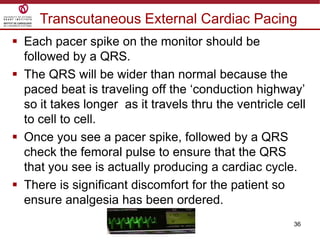
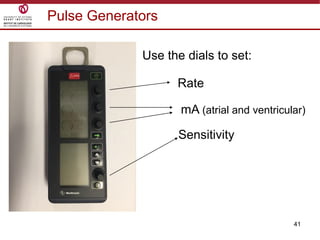
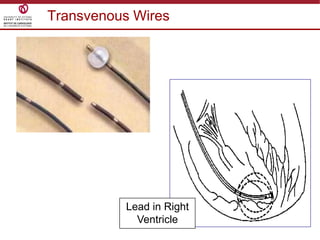
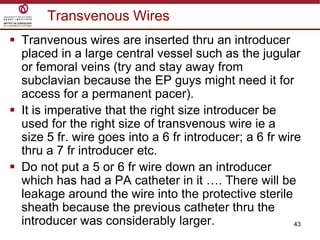
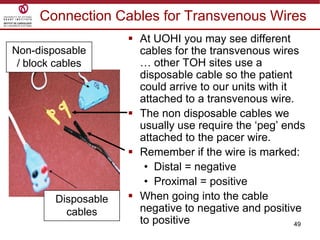
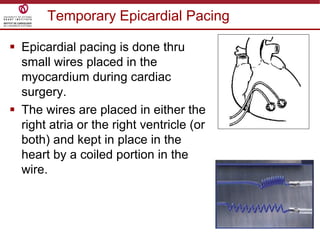
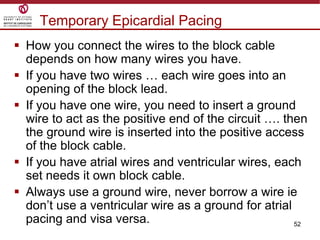
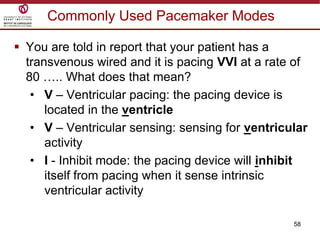
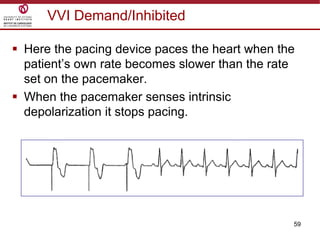
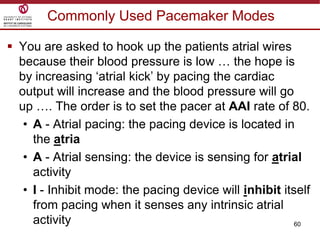
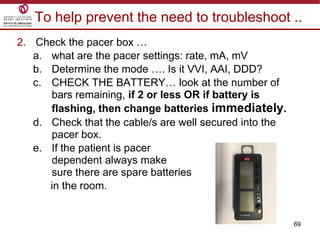
Temporary cardiac pacing is used when a patient's heart rate is too slow or irregular. There are three main types: transcutaneous pacing using pads on the chest, transvenous pacing using a wire inserted into the heart via a vein, and epicardial pacing using wires placed during cardiac surgery. The pacing method depends on urgency and availability. A pulse generator is attached to the pacing wires and is used to deliver electrical impulses and adjust settings like rate, amplitude, and sensitivity. The goal is consistent capture of the heart without unnecessary pacing.