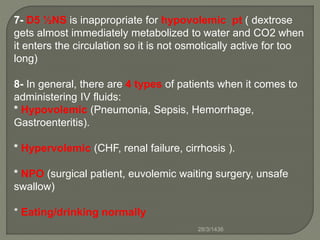
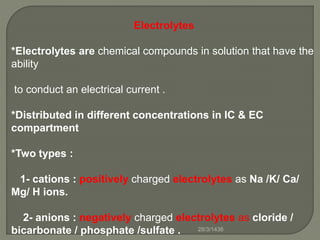
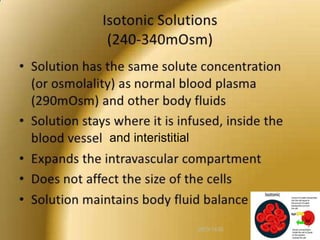
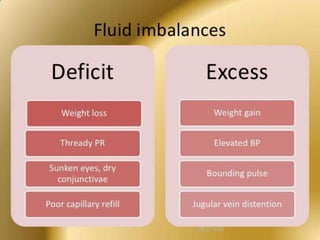
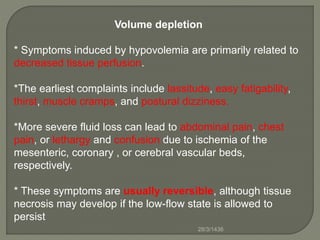
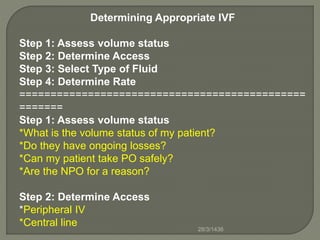
1) Intravenous fluid therapy is used to treat fluid imbalances and electrolyte abnormalities. It involves determining the appropriate rate and type of intravenous fluid based on a patient's volume status, electrolyte levels, and ongoing losses or gains.
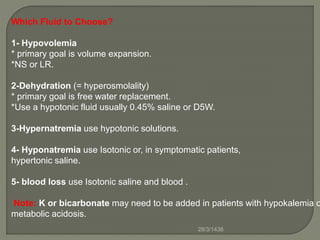
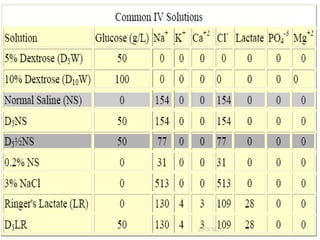
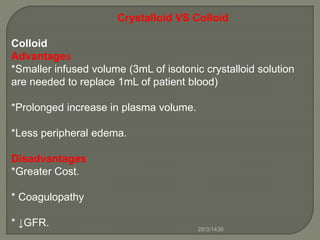
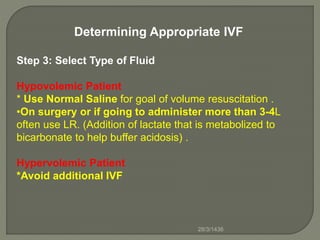
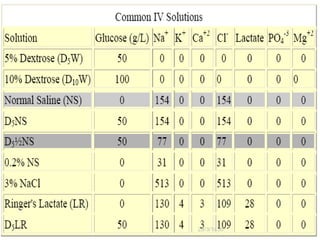
2) Common types of intravenous fluids include crystalloids like normal saline and lactated Ringer's, which are used for volume expansion, and colloids, which increase vascular volume more rapidly but are more expensive.
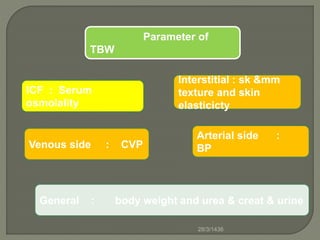
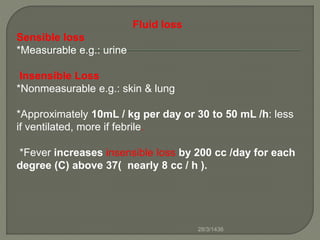
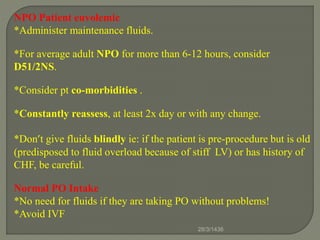
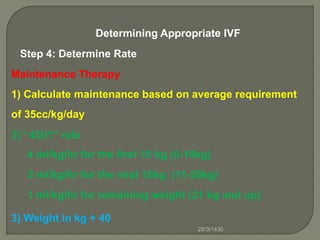
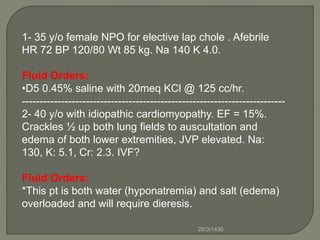
3) Maintenance intravenous fluids are given to replace normal daily losses when a patient cannot take fluids orally, while replacement fluids are used to correct existing dehydration or volume deficits based on parameters like blood pressure, jugular pressure, and urine output.
































![Hypernatremia
Rate of fluid administration mL /h = water deficit x 10 ÷ (serum Na -
140)÷ 24
+
Obligatory water output from sweat and stool, which is approximately
30 to 40 mL /h.
*Rate of lowered serum sodium per day =10 meq /L per day
*The water deficit should be replaced over at least (serum Na -140) ÷ 10
= days, or day/24 = hours
*Obligatory water output from sweat and stool, which is approximately
30 to 40 mL /h.
Serum [Na]
*Water deficit = Current TBW x (——————— - 1)
140
*Current TBW= W X male 60% or female 50%28/3/1436](https://image.slidesharecdn.com/meeting-copy-150317141127-conversion-gate01/85/IVF-46-320.jpg)
![Hyponatremia
1)Na deficit (total needed) = Current TBW x (desired Na -
serum Na)
2) desired rate/hr = Amount needed to increase serum
level by 0.5 meq/L/hr = Current TBW x 0.5
3) 3% hypertonic saline contains 513 meq /Liter
[desired rate/hr]/513 x 1000 = ml/hr
4) Length of infusion = Na deficit / desired rate/hr =
hours
28/3/1436](https://image.slidesharecdn.com/meeting-copy-150317141127-conversion-gate01/85/IVF-47-320.jpg)


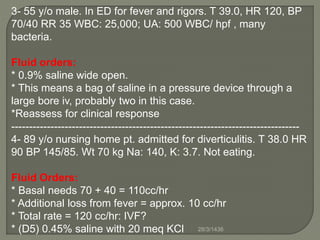
![5-50 y/o with massive hematemisis, SBP 80 HR 130 IVF?
Fluid Orders:
* 0.9% saline WIDE OPEN through two large bore IVs.
*O neg STAT
*Type and cross 6 units PRBC STAT
-------------------------------------------------------------------------
6-65 y/o male hospitalized with pneumonia. Temp 38.5, HR 72,
BP 125/72. Wt 75 kg. Na:165 K: 4.0.
Fluid Orders:
*Basal needs 115 cc/hr + 12 cc/hr for fever.
Also:
* Free water deficit of (.6)(75)[(165/140) – 1] =
7.6 liters.
* IV # 1: 0.45% saline @ 130 cc/hr.
* IV # 2: D5W @ 150cc/hr for 50 hrs.
28/3/1436](https://image.slidesharecdn.com/meeting-copy-150317141127-conversion-gate01/85/IVF-57-320.jpg)