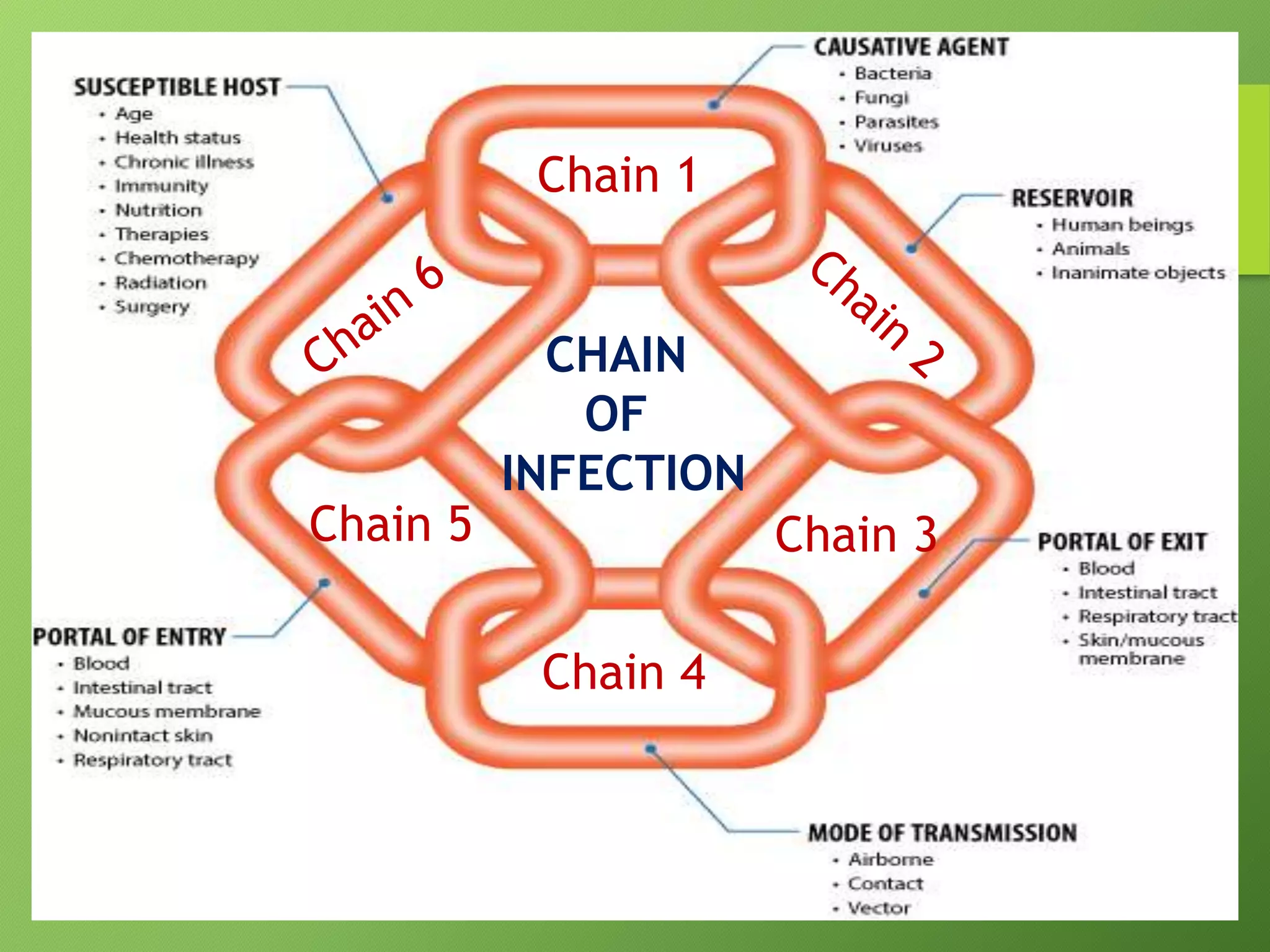
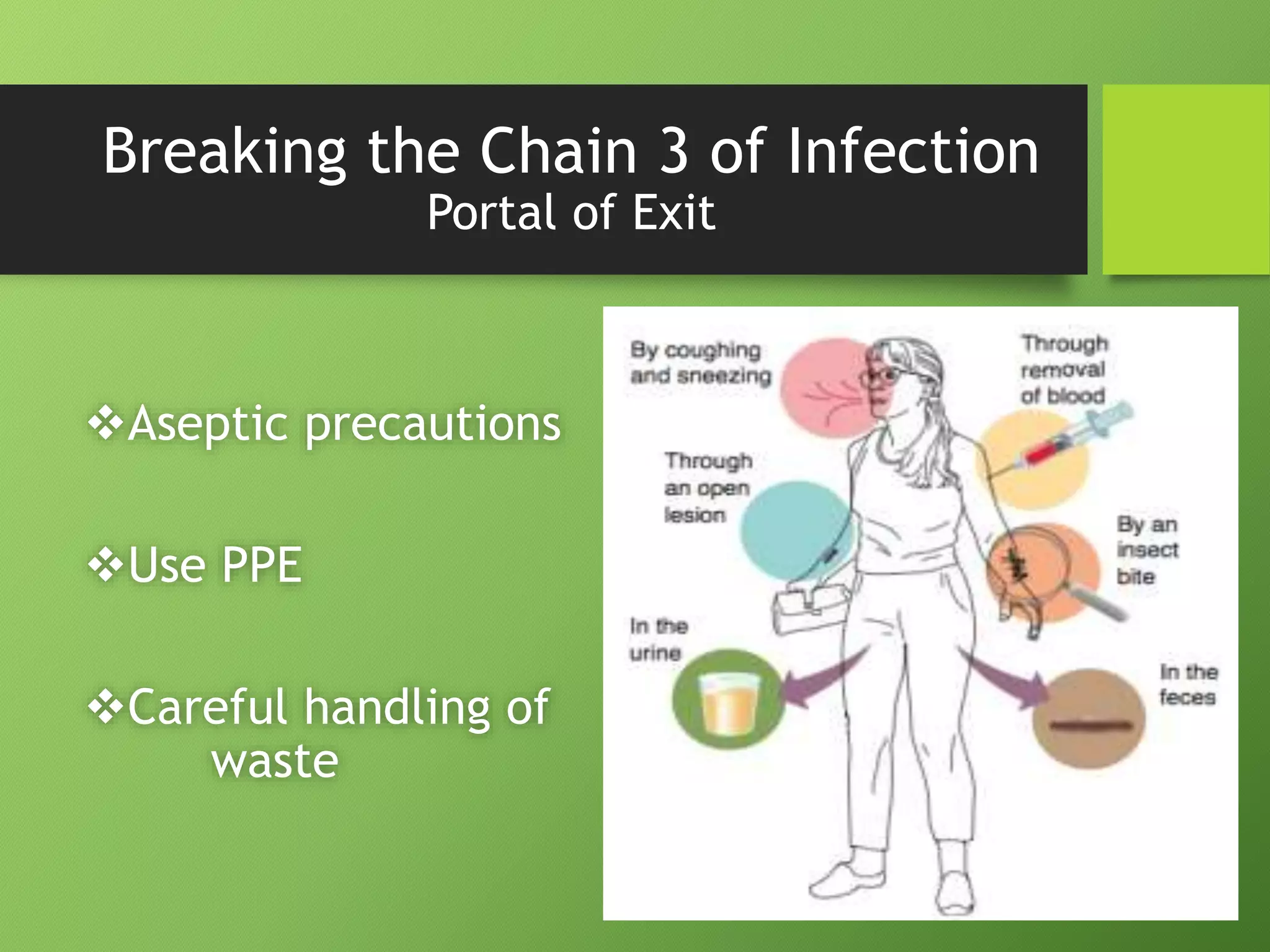
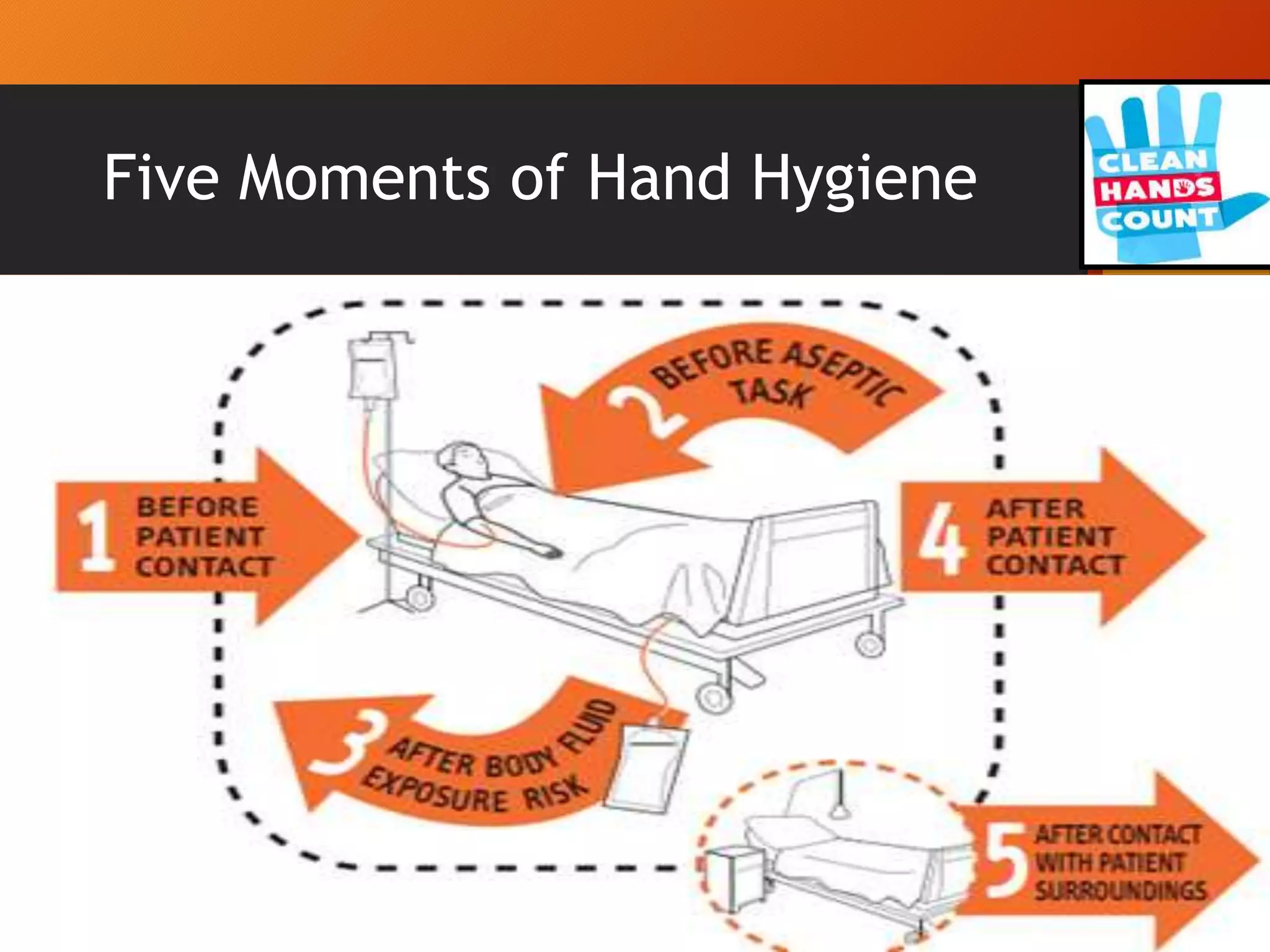
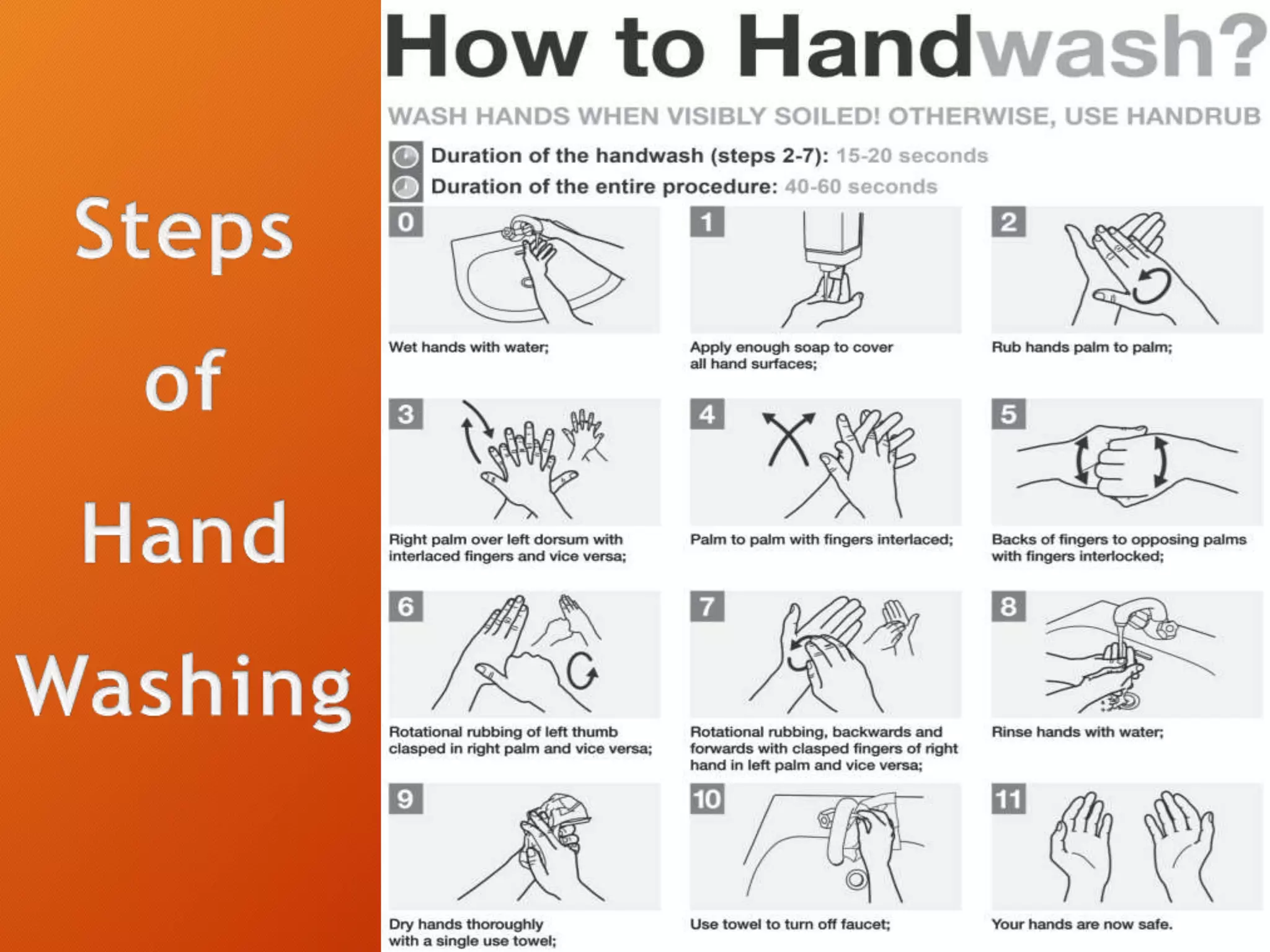
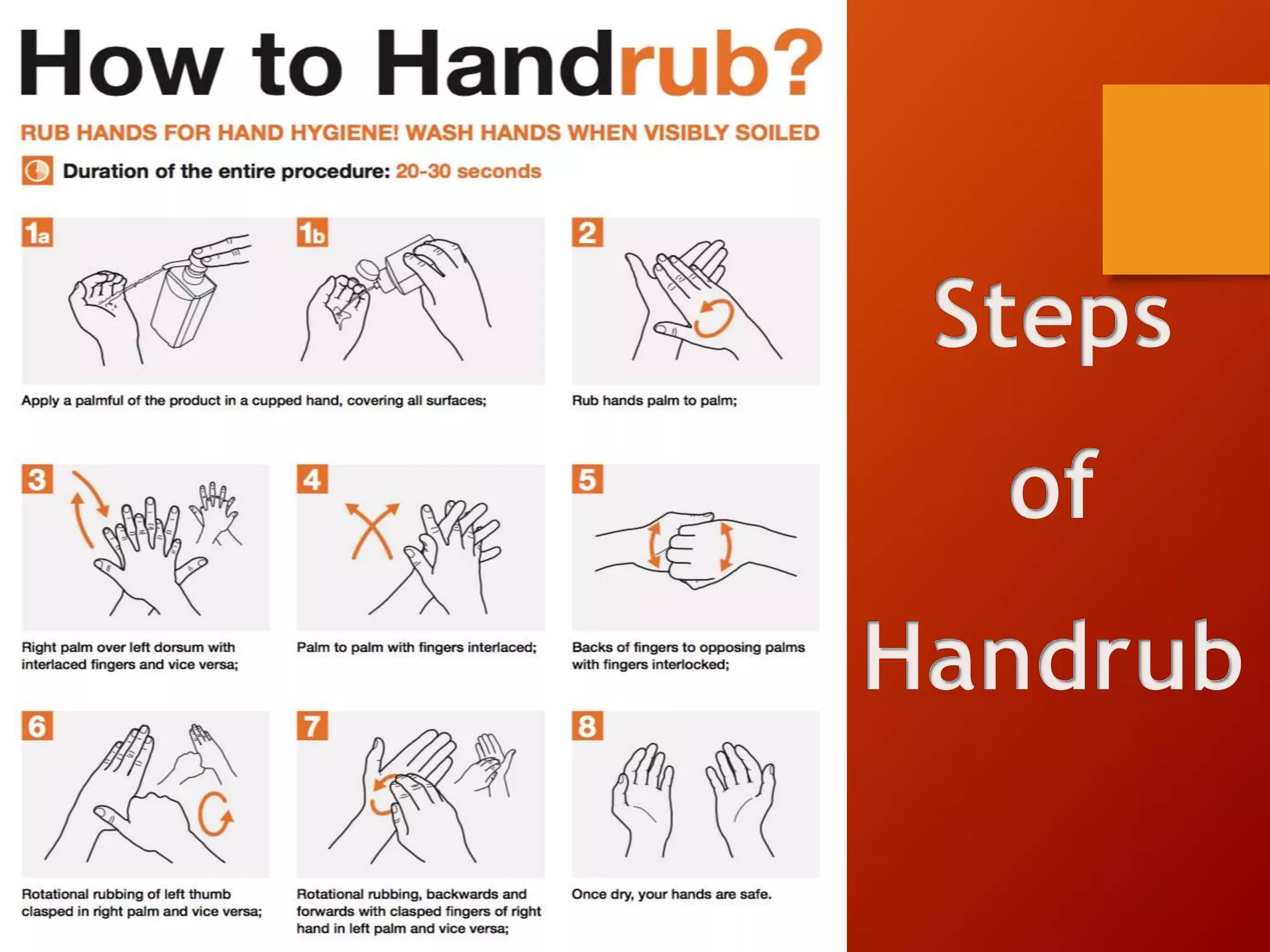
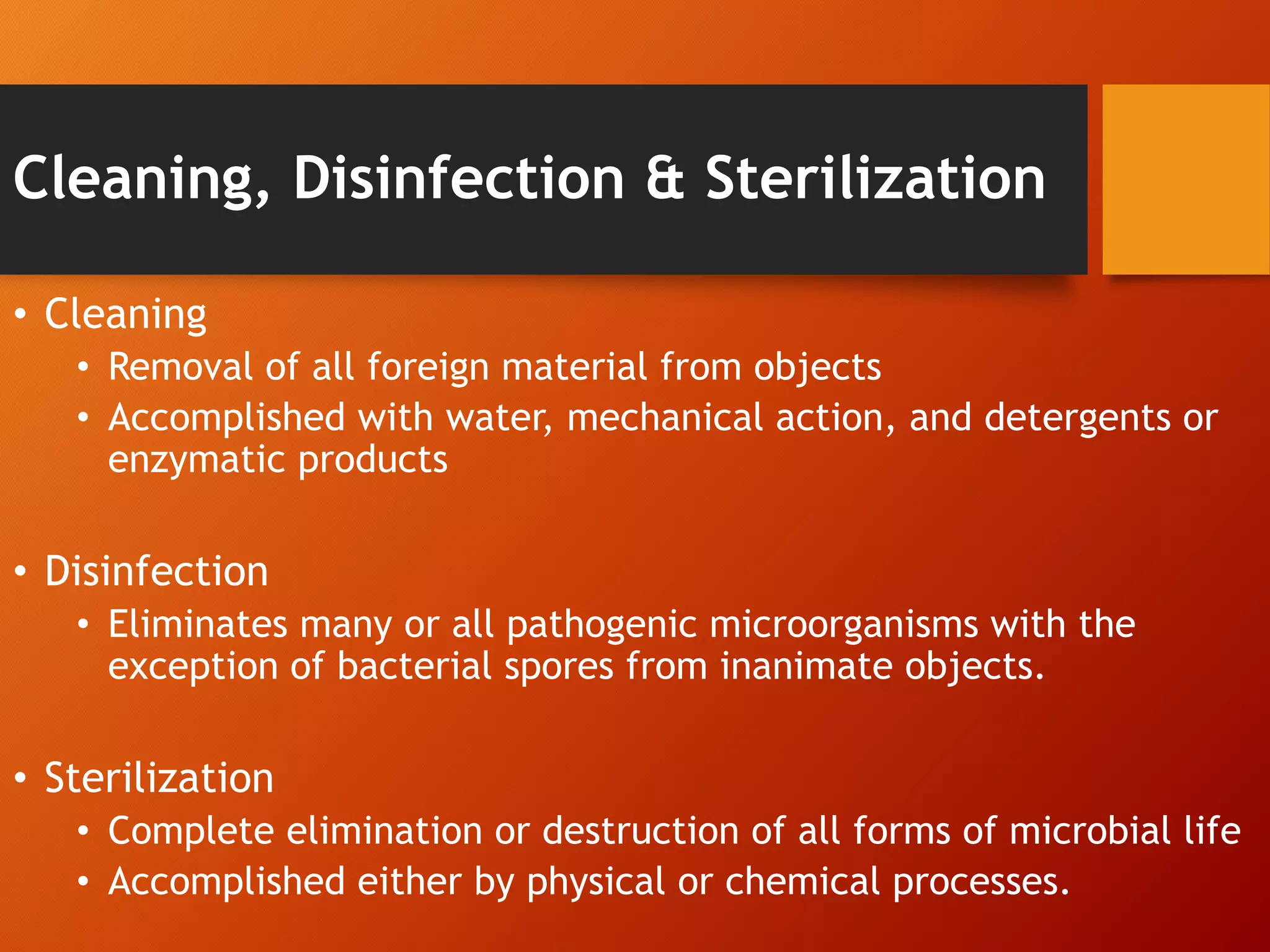
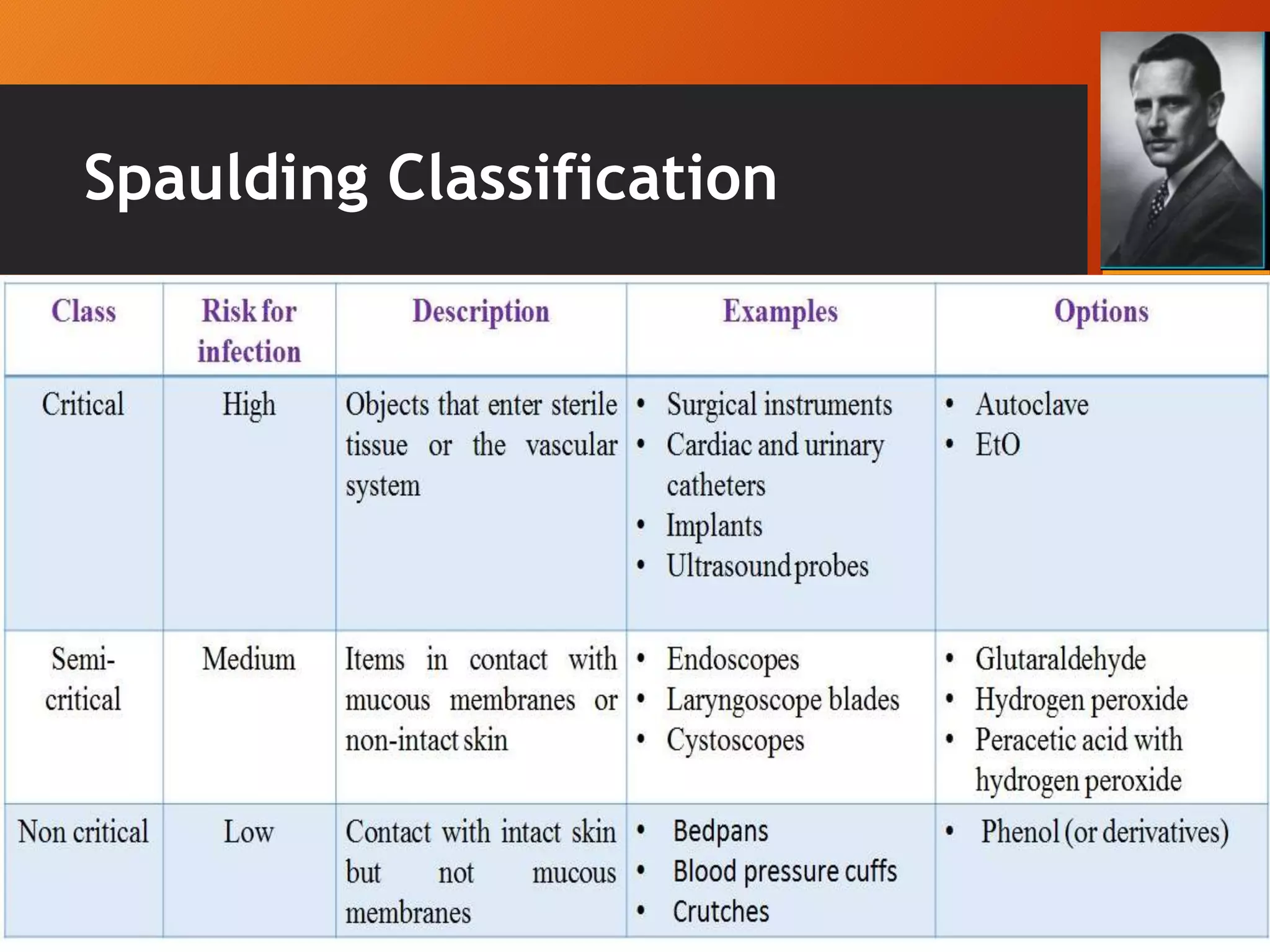
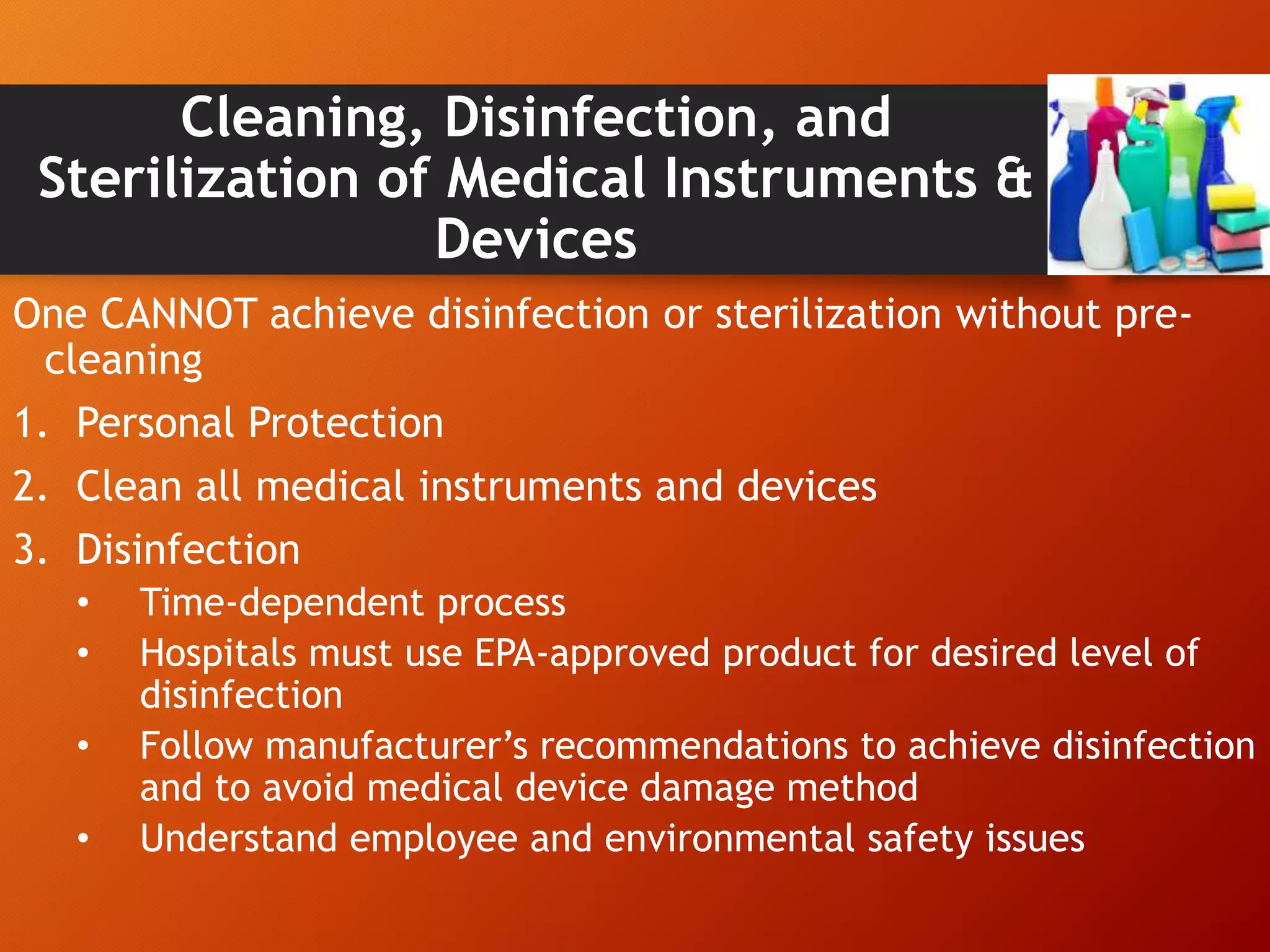
The document discusses infection control and standard safety measures in healthcare facilities. It covers topics like infection control programs, the chain of infection, hand hygiene, personal protective equipment, needlestick injury prevention, environmental cleaning, cleaning and sterilization of medical equipment, biomedical waste management, safe injection practices, and the roles and responsibilities of hospital infection control committees. The overall aim is to prevent healthcare-associated infections and protect both patients and healthcare workers from infections.