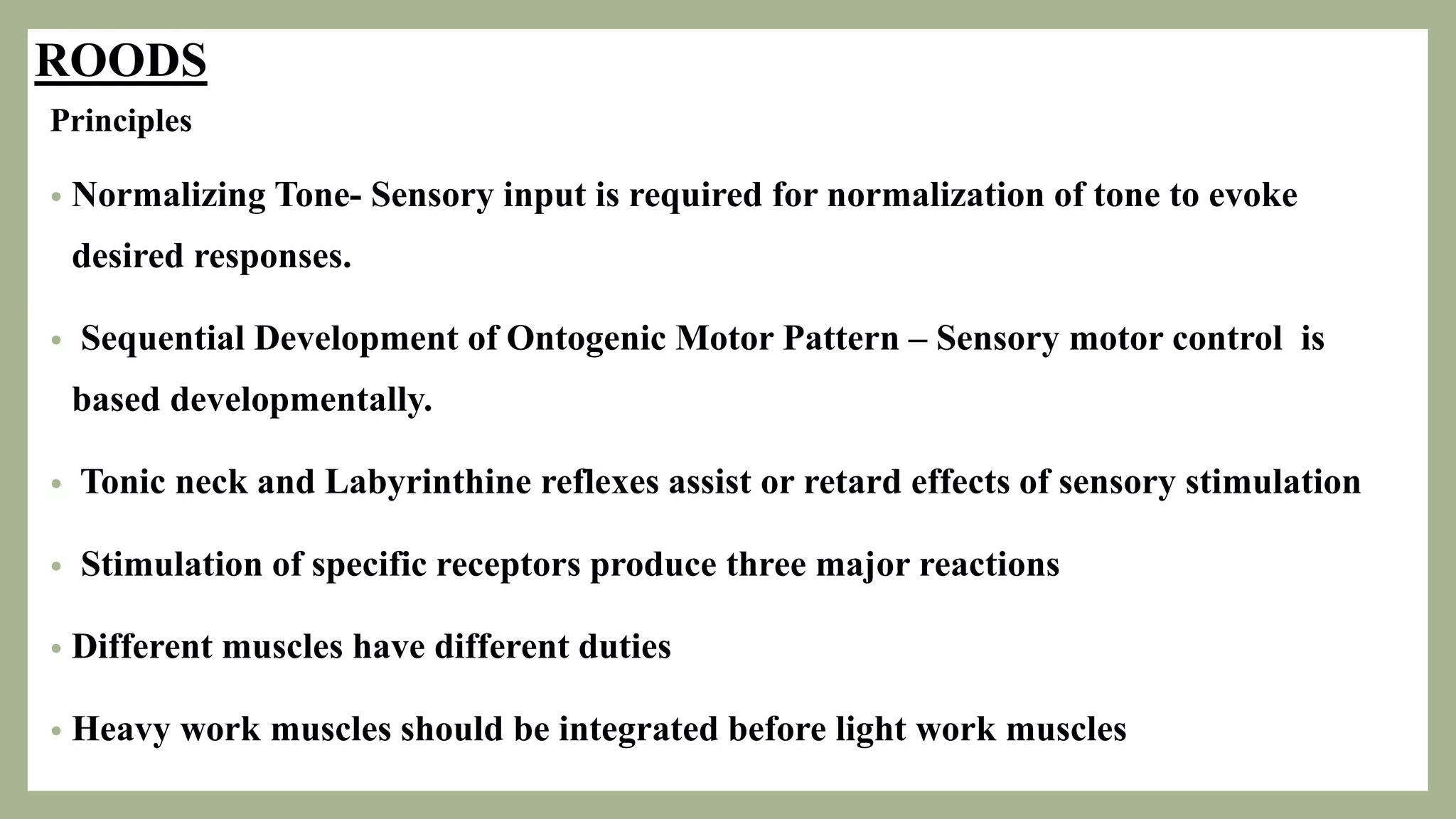
The document outlines various neurological therapy approaches and their applications in managing disorders and diseases. It details principles and techniques of methods such as proprioceptive neuromuscular facilitation, neurodevelopmental therapy, and constrained induced movement therapy, emphasizing individualized patient treatment. Recent advances are integrated with classic approaches, highlighting the importance of neuroplasticity, motor learning, and collaborative care in enhancing patient outcomes.







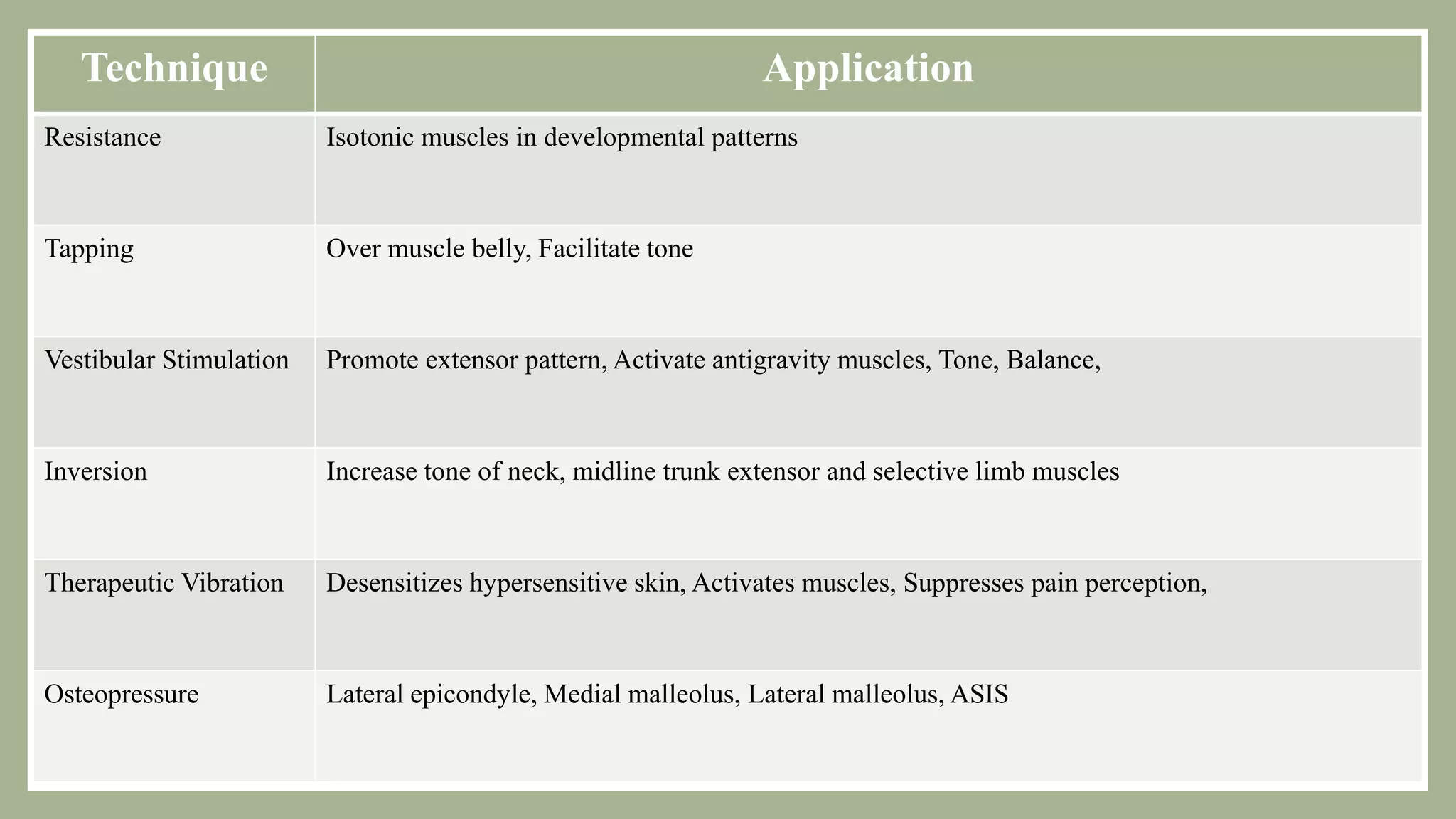










![B] Sensory stimulation Techniques
- Sensory diet
- Swinging
- Floor time
- Snoezelen room intervention(Controlled
multisensory ENV)
- Animal assisted therapy
- Sensory garden
- Play skills
- Sensory based Intervention – Single
Sensory or Multisensory
A] Sensory stimulation Protocols :
- Wilbarger Protocol
- Astronaut Program
- Brain gym activities
- Miller method
- Reciprocal imitation training](https://image.slidesharecdn.com/neurologicalapproaches-230717144114-67330233/75/Neurological-Approaches-25-2048.jpg)