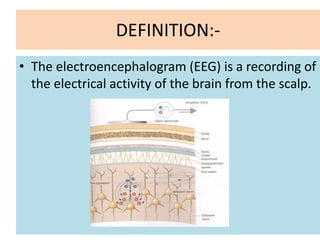
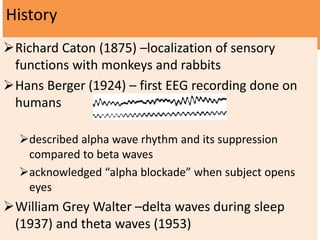
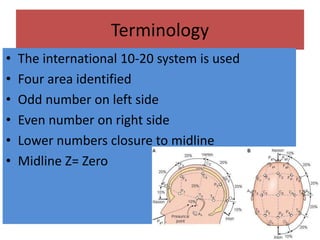
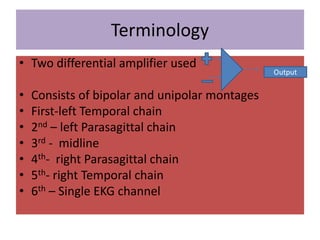
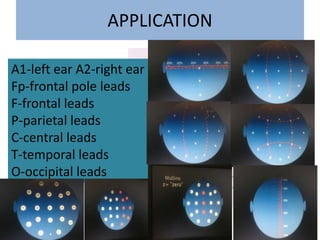
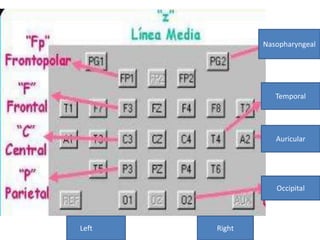
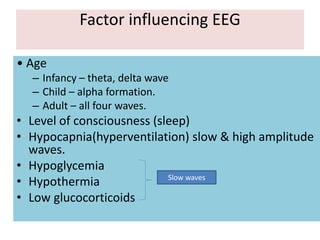
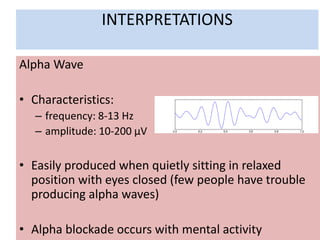
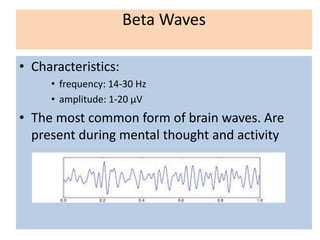
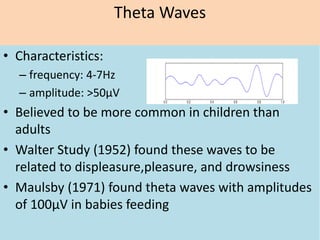
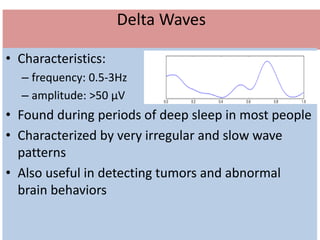
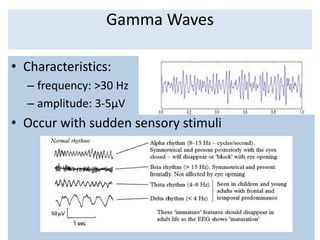
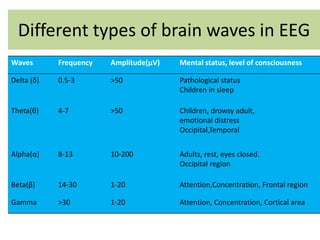
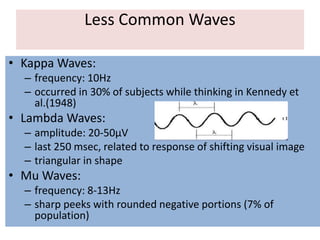
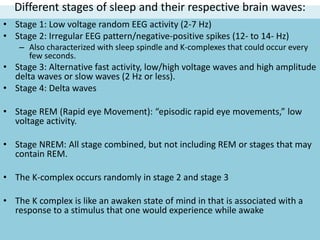
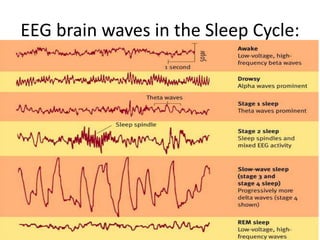
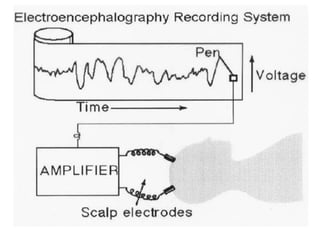
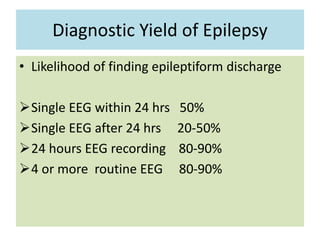
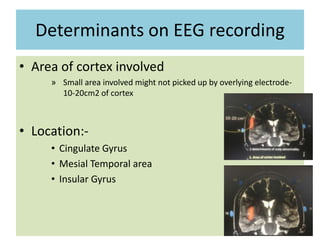
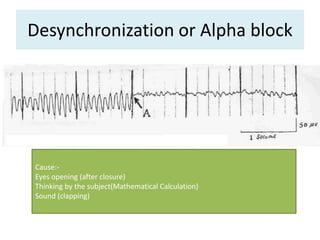
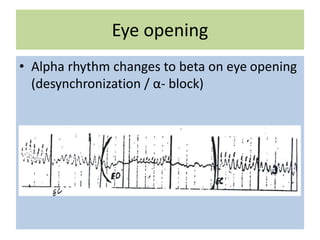
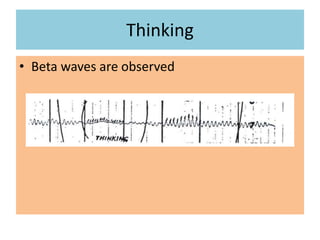
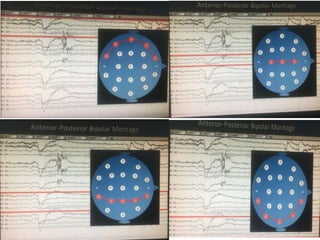
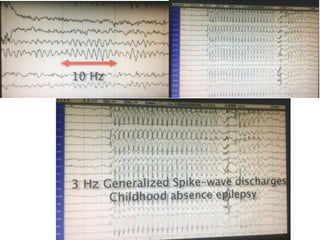
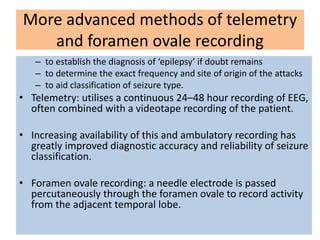
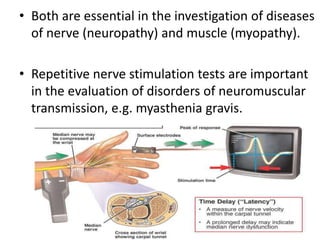
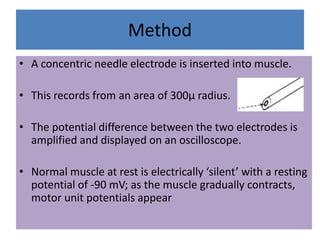
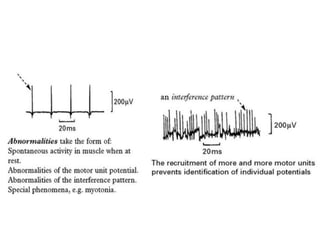
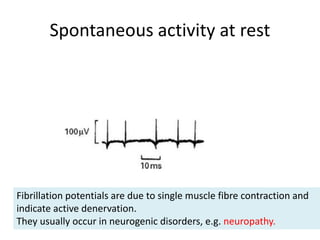
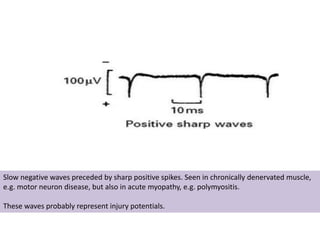
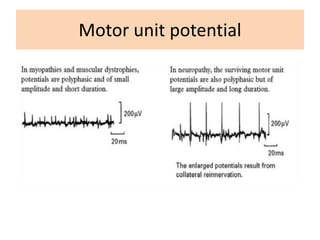
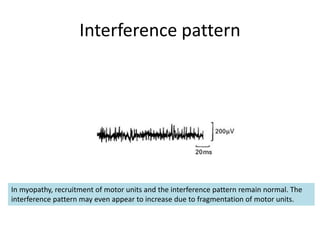
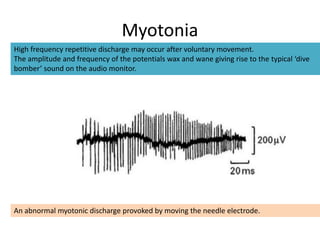
The document provides information about EEGs and EMGs. It defines EEG as recording electrical activity of the brain from the scalp and notes its history and applications in diagnosing conditions like epilepsy. It describes different brain waves seen in EEGs including alpha, beta, theta, and delta waves and their characteristics. It also summarizes sleep cycles and brain waves associated with each stage of sleep. The document then discusses EMG and how it records muscle activity through motor units. It notes the techniques of surface EMG and intramuscular EMG and what abnormalities in spontaneous activity or motor unit potentials can indicate.