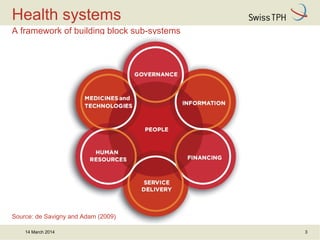
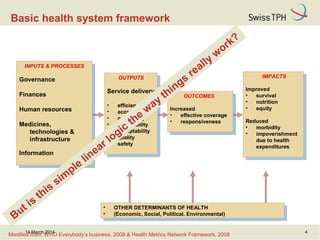
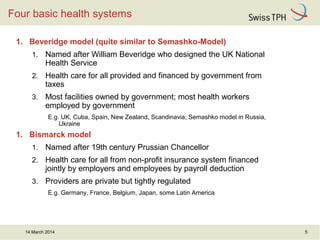
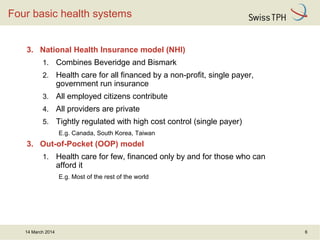
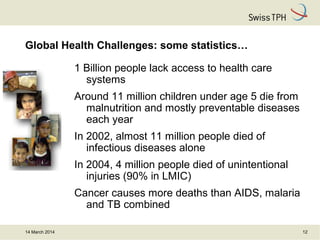
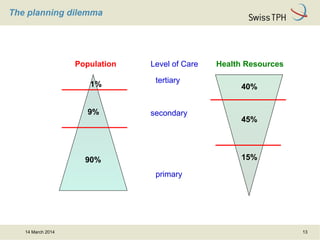
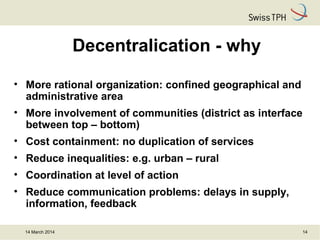
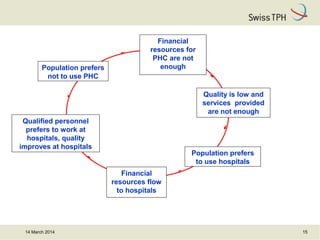
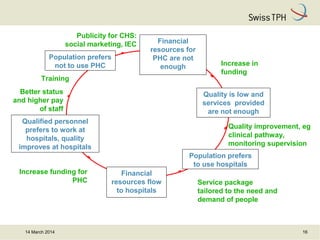
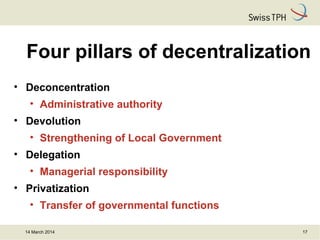
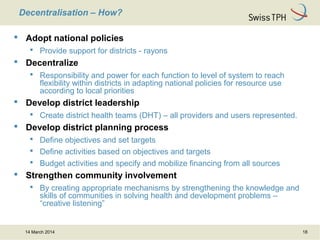
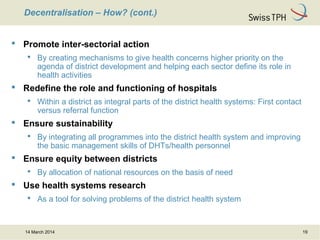
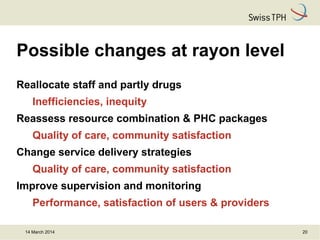
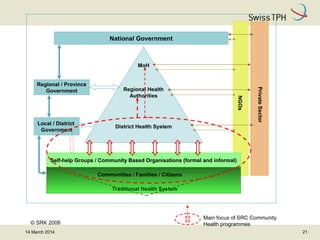
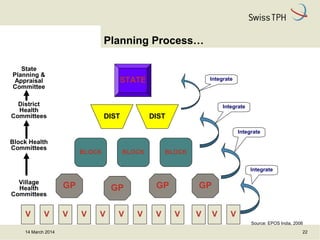
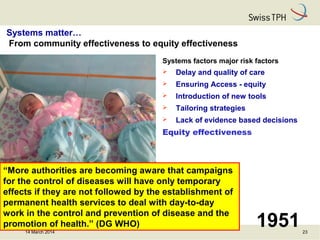
The document discusses the challenges and frameworks of health systems, focusing on the efficacy of decentralization in healthcare delivery. It covers various models such as Beveridge, Bismarck, National Health Insurance, and Out-of-Pocket models, highlighting their impacts on equity and quality. Additionally, it emphasizes the significance of decentralization in improving healthcare accessibility and solutions for global health challenges.