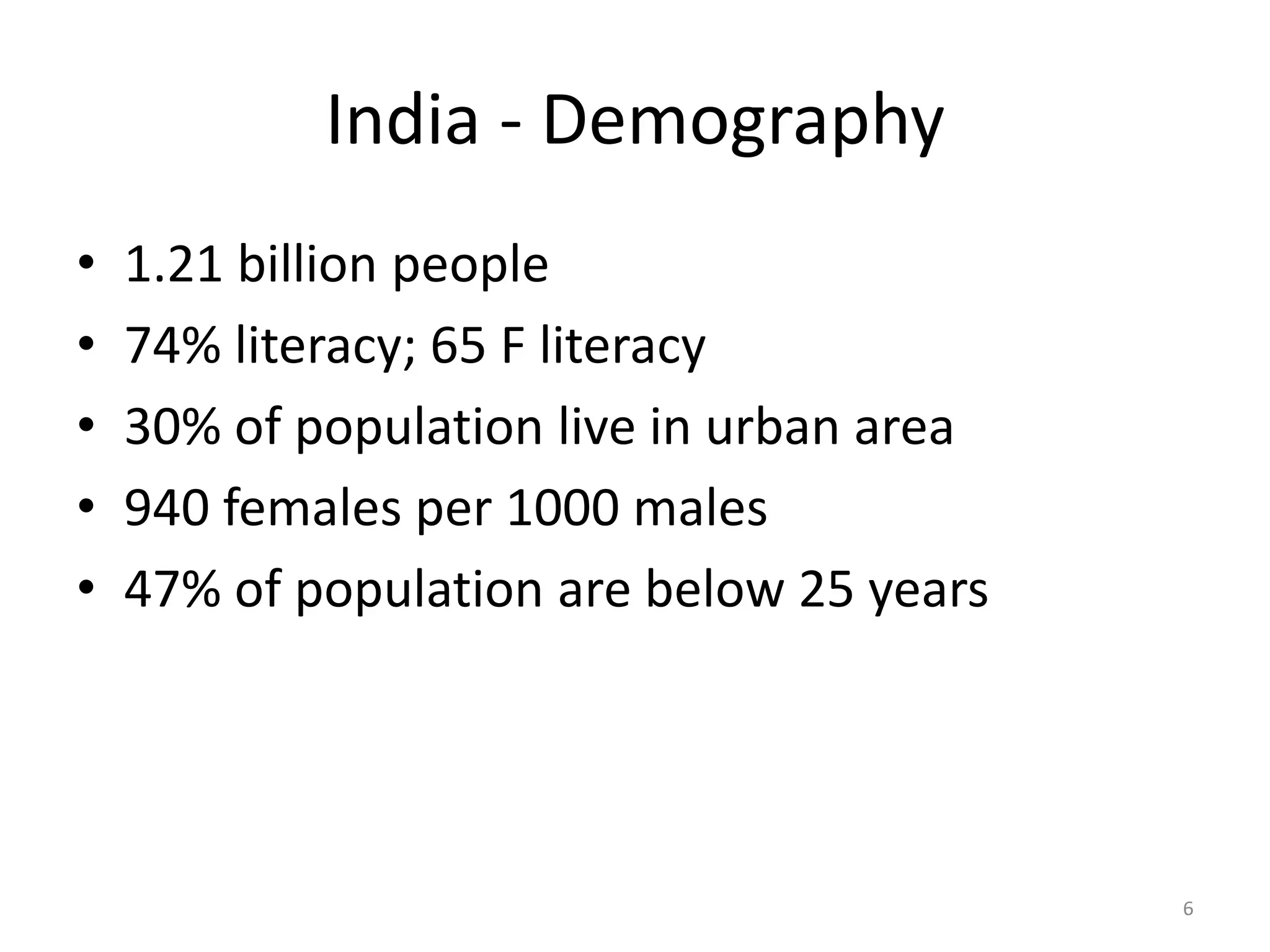
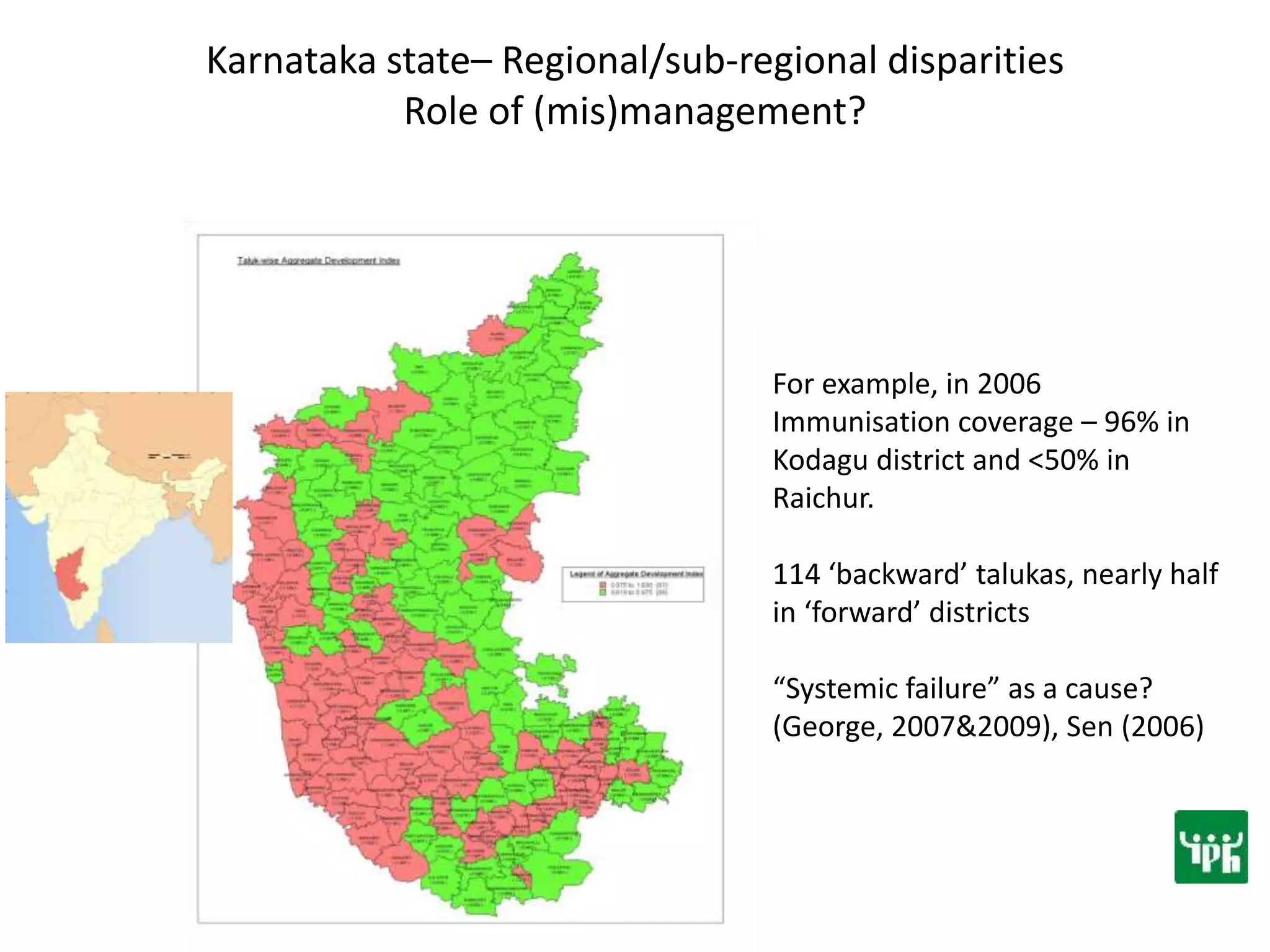
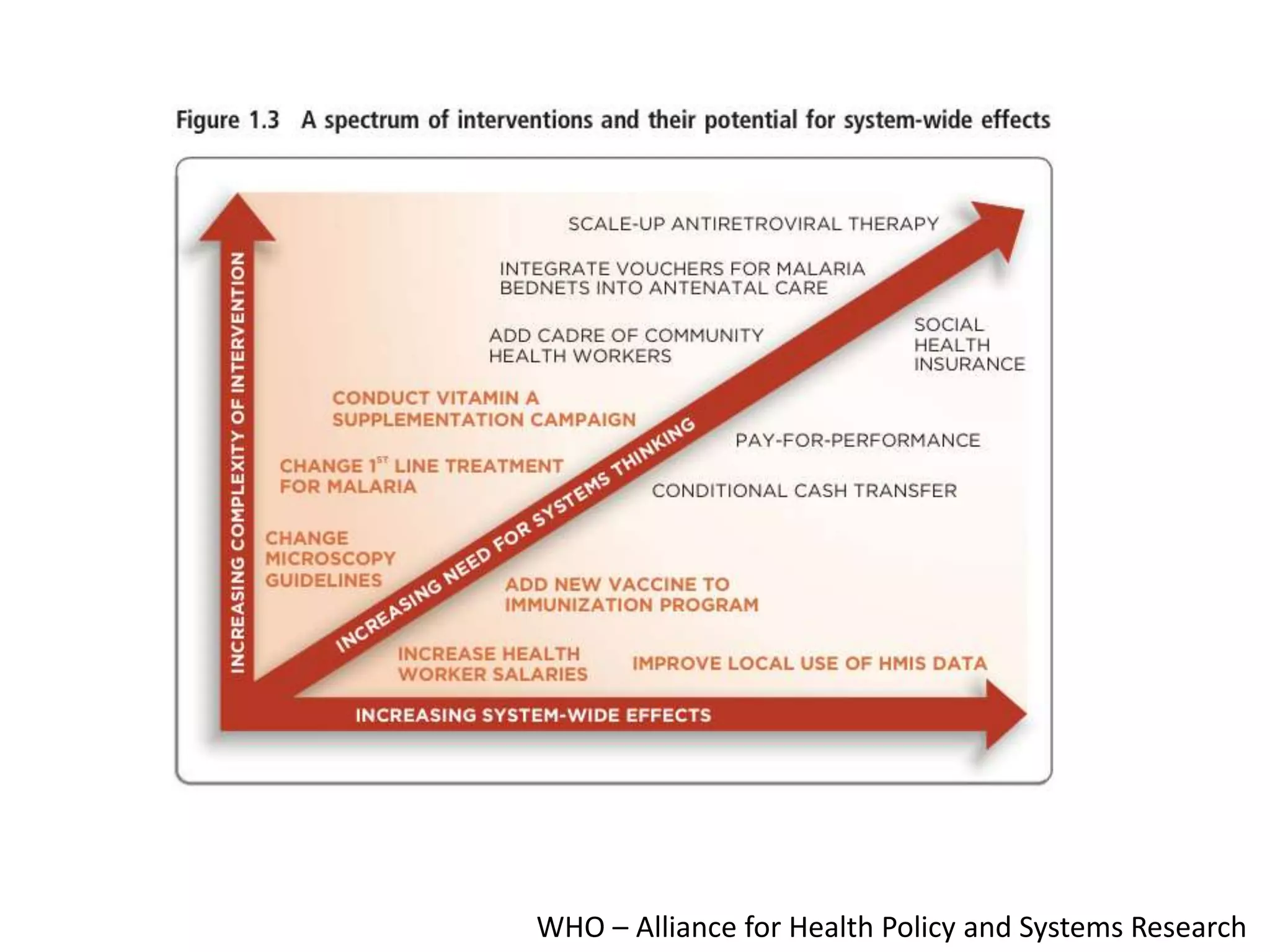
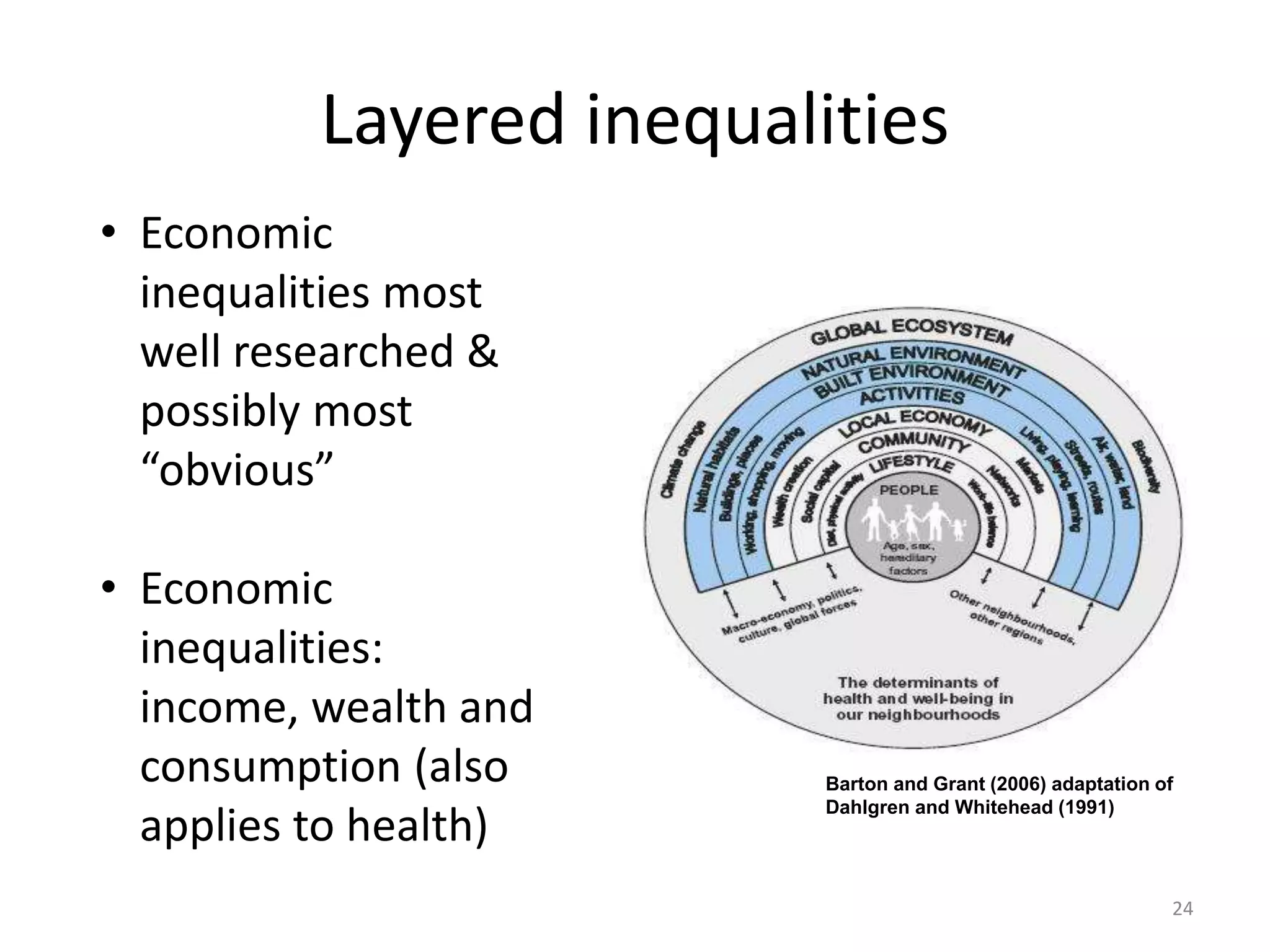
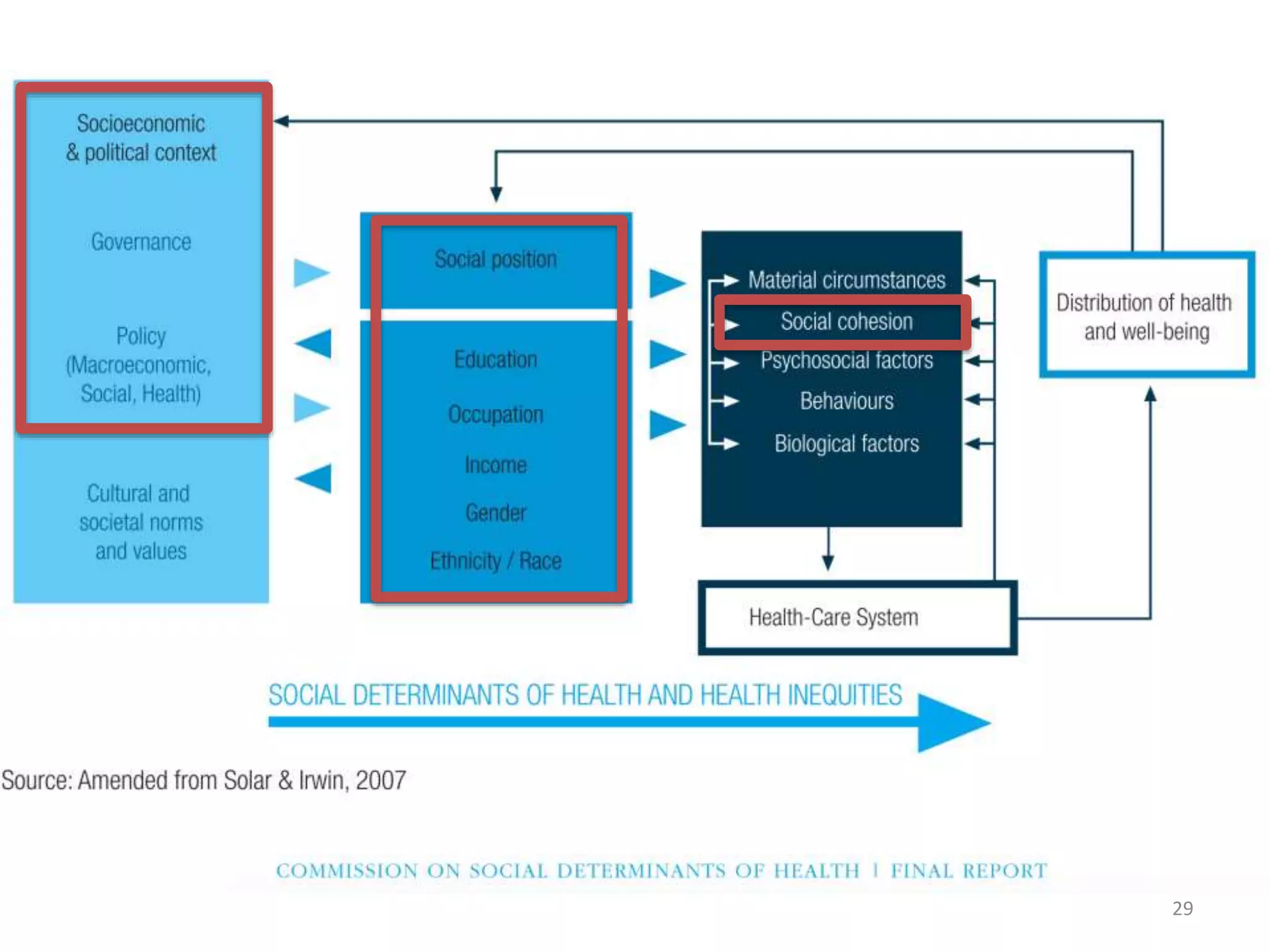
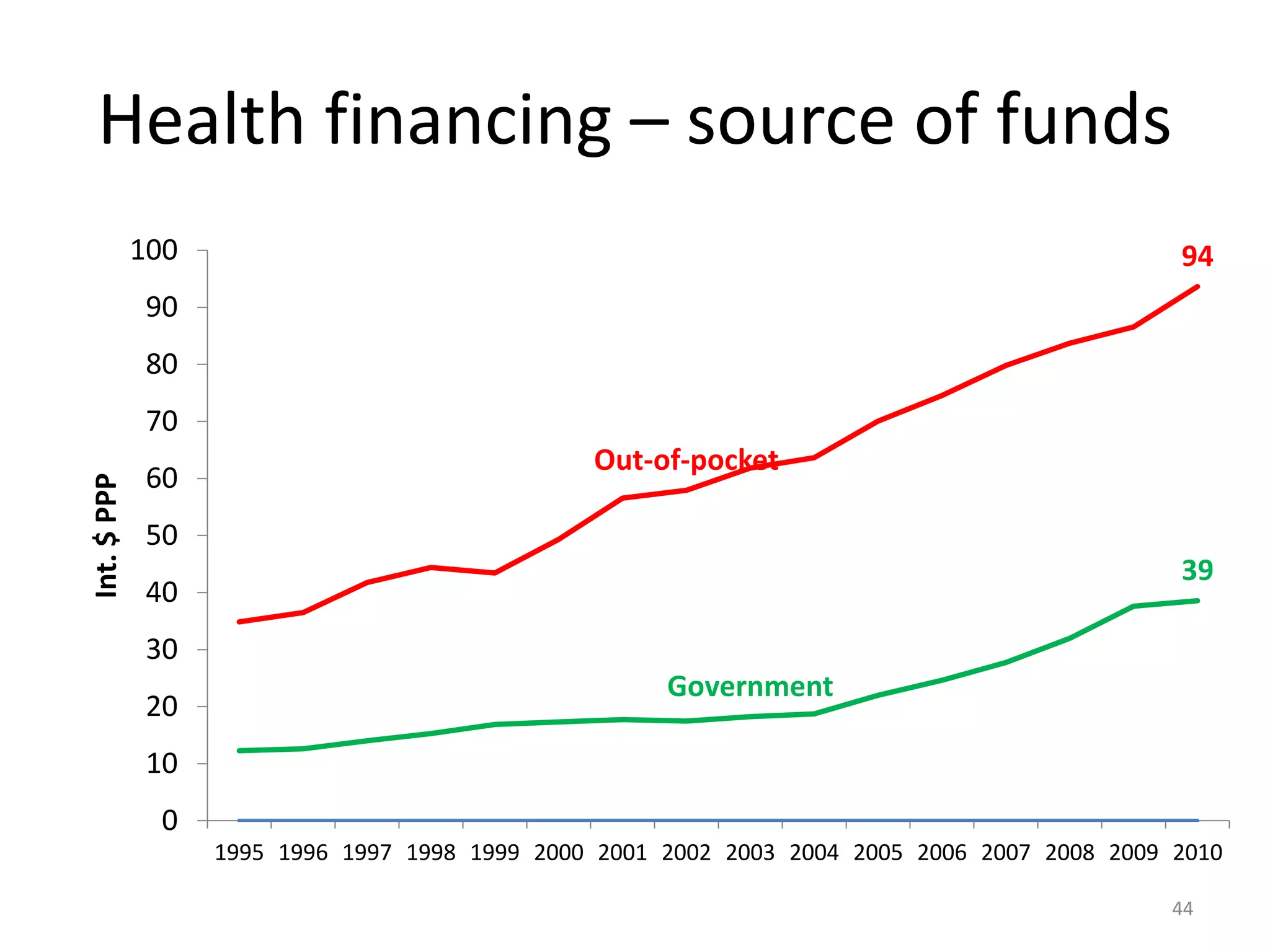
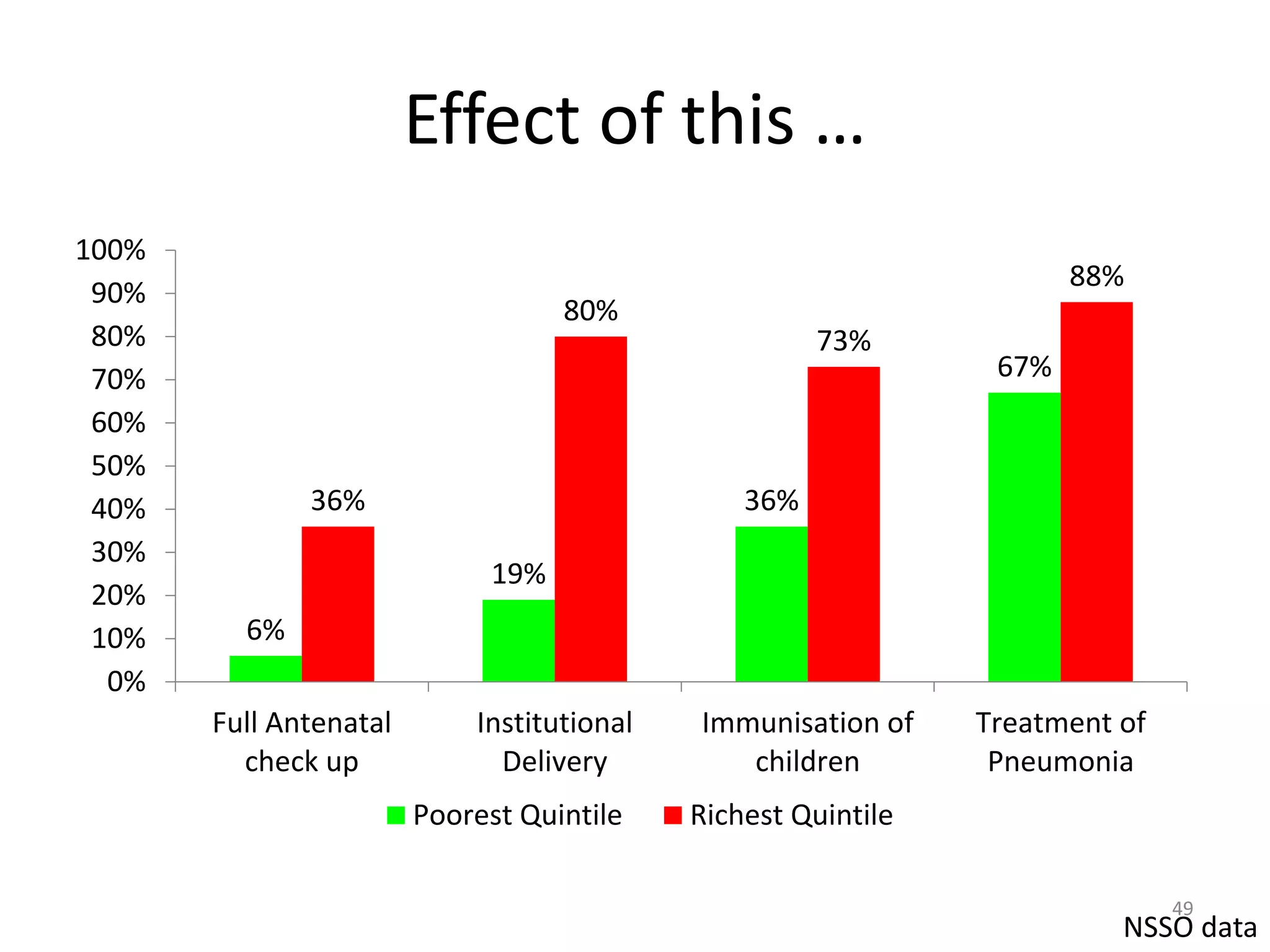
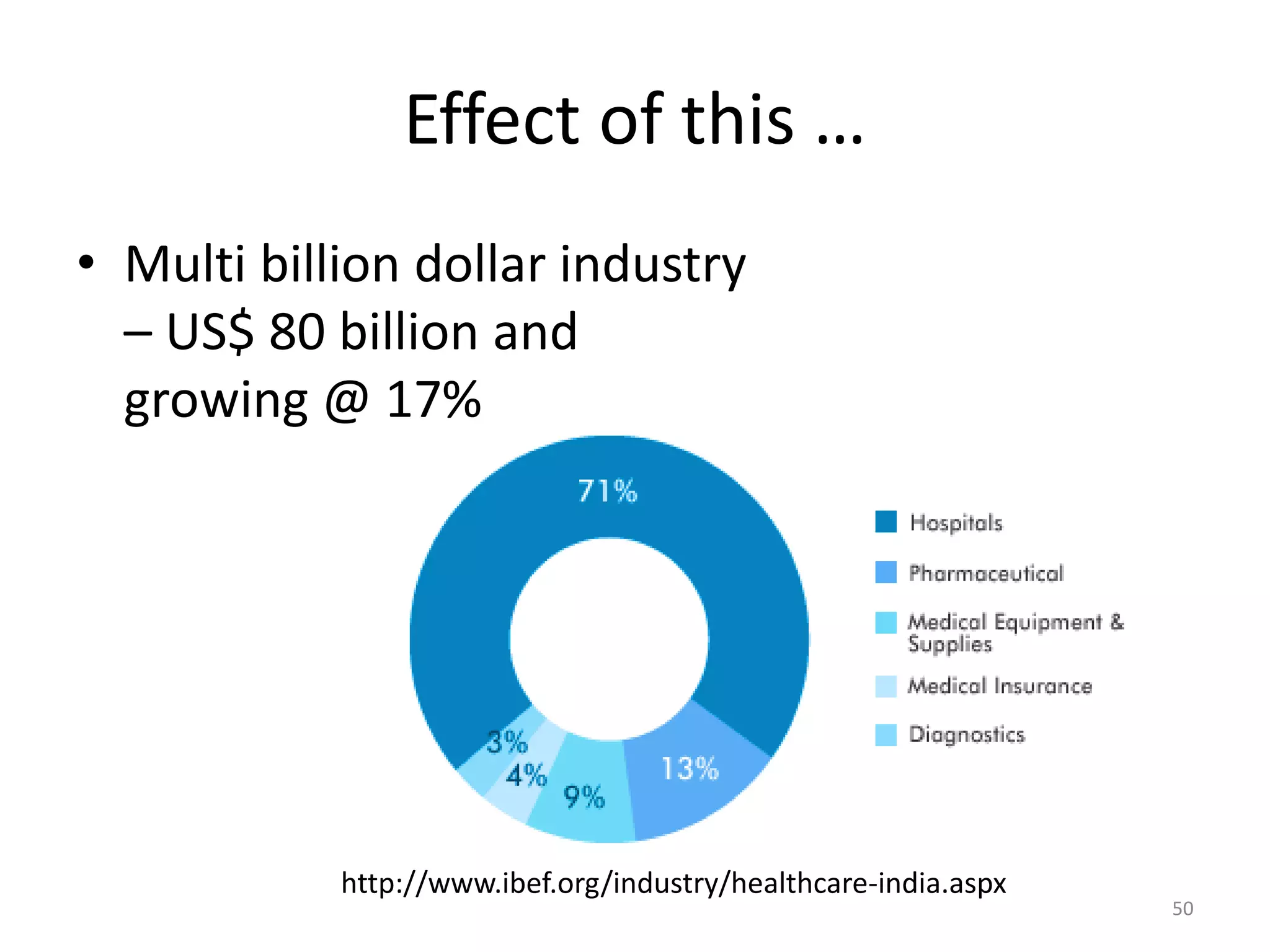
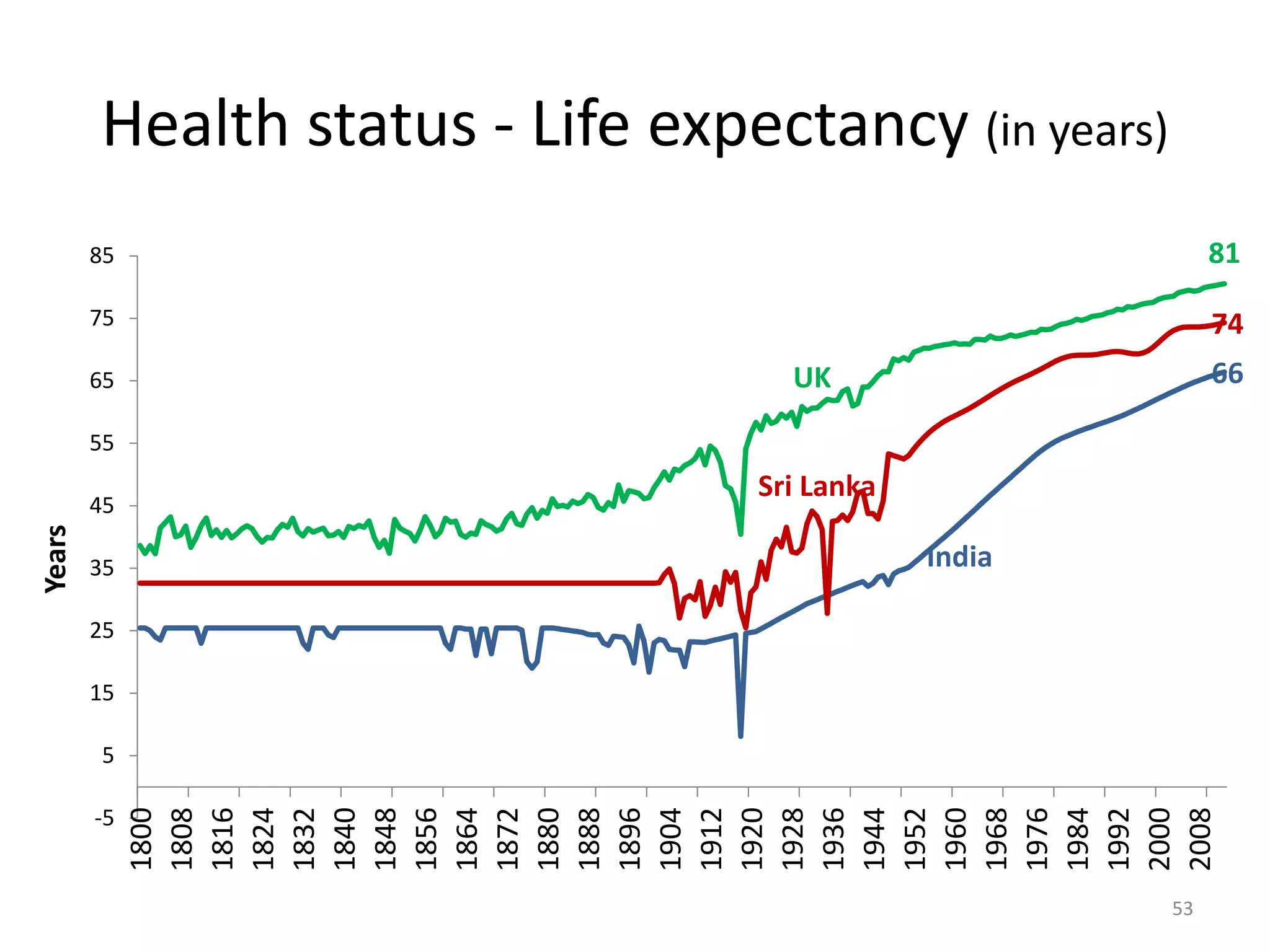
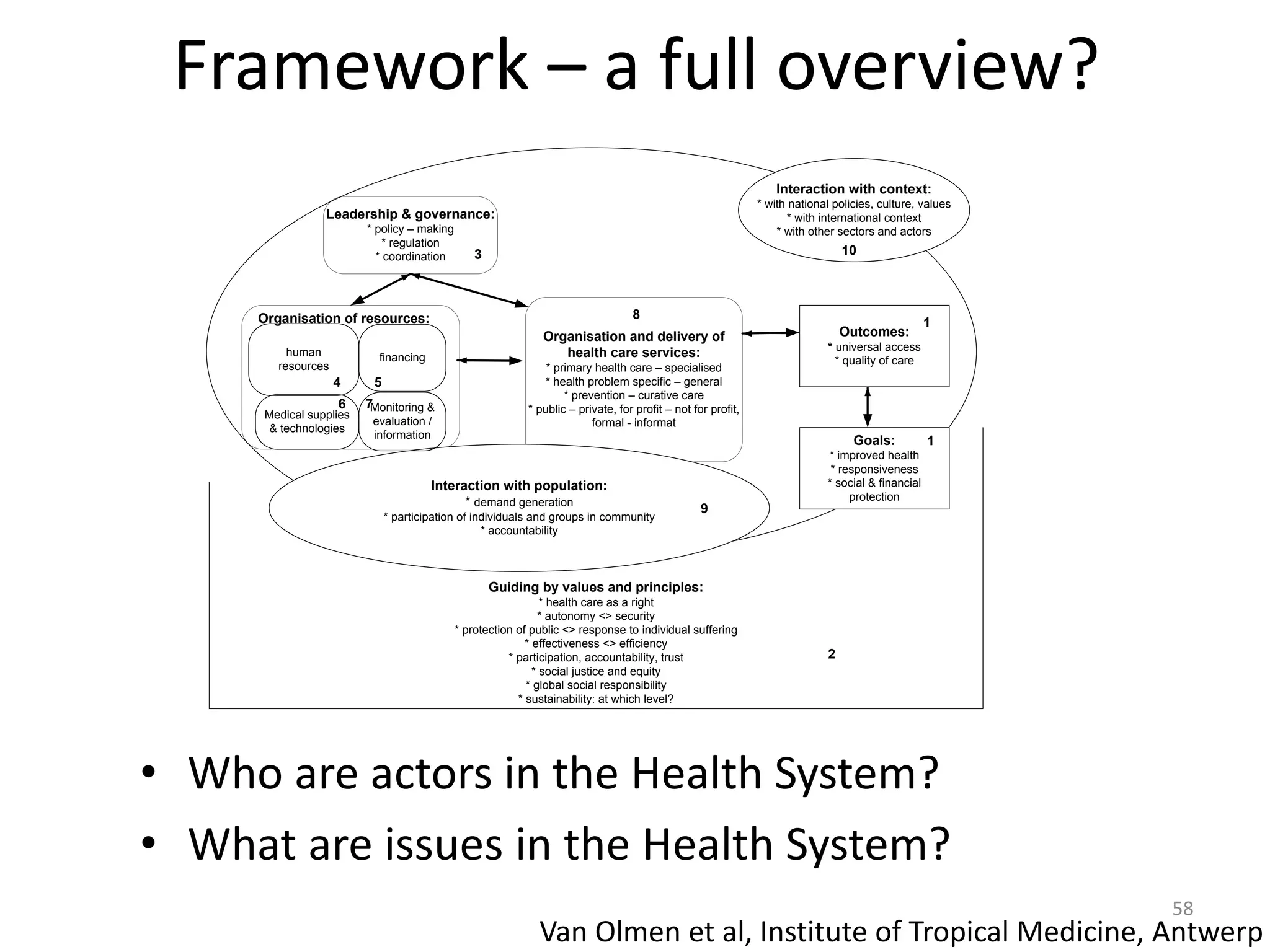
The document provides an overview of the Indian health system, addressing issues such as healthcare inequity, human resource challenges, financing models, and the dual burden of communicable and non-communicable diseases. It highlights the complex landscape of health services in India, characterized by a strong private sector and significant out-of-pocket expenses for patients. The analysis includes social determinants of health and the need for improved governance and efficiency in health expenditure by the government.